Peer Reviewed References:
Excerpts from Peer-Reviewed Mini Dental Implant Studies that extol their virtues for a viable option of replacing & restoring single to multiple missing teeth in a minimally invasive and more affordable way.
Dennis Flanagan; Rationale for Mini Dental Implant Treatment.
J Oral Implantol
1 October 2021; 47 (5): 437–444.
doi: https://doi.org/10.1563/aaid-joi-D-19-00317
“Mini dental implants can be used to support crowns and partial and complete dentures in compromised edentulous sites. Lack of bone width or site length may be treated with mini implants. Mini implants have less percutaneous exposure and displacement that may reduce complications. Nonetheless, mini implants transmit about twice the load to the supporting bone, and thus, control of occlusal loading is important.”
MDI ClinicalStudies from AroundTheUSA
Boston,Massachusetts 2012
How Successful are Small Diameter Implants: A Literature Review 2012
Keyvan Sohrabi Ammar Mushantat Shahrokh Esfandiari Jocelyne Feine
Keyvan Sohrabi, Deptartment of Oral Health Policy and Epidemiology,
Harvard School of Dental Medicine, Boston, MA, Clin. Oral Impl. Res. 0, 2012 / 1–11
© 2012 John Wiley & Sons A/S
https://www.dentatususa.com/
fileadmin/user_upload/PDF/
PDF_Reference
_Articles/114_Jan_2012_Sohrabi.pdf
Abstract
Background:
Edentulism is an important issue and will remain so due to high numbers of edentate individuals worldwide. For many years, complete dentures have been the only treatment option for this population. Implant overdentures have been shown to have many advantages over conventional complete dentures. However, although dissatisfied with their mandibular dentures, some edentate elders are reluctant to undergo even simple implant treatment due to factors such as cost and fear of surgery. To address these obstacles, this paper reports on a review of small- diameter implant (SDI) studies that were performed in the last two decades. The aim of this study is to (i) determine the survival of narrow diameter implants, (ii) determine whether survival is dependent on whether these implants are placed using a flap or flapless approach, and (ii) determine whether there is a relationship between length and implant survival in SDIs.
Methods:
In this review, studies were included that (i) involve implants with 3.5 mm diameter or less, (ii) have a randomized clinical trial, retrospective or prospective cohort design with human subjects, (iii) provide a follow up duration of at least 5 months following implant placement, (iv) include data on the survival rate of the implants.
Results:
Forty one studies meeting the above criteria were published between 1993 and 2011 using SDIs from a variety of companies and surface characteristics with diameters of 1.8 mm to 3.5 mm and lengths of 8 mm to 18 mm. A total of 10,093 SDIs were inserted in approximately 2762 patients. Twenty-six studies involved flap reflection techniques for implant placement, six studies used a flapless technique and two studies used both techniques; in the remaining studies, the technique was not specified. Follow up duration varied from 5 months to over 9 years. The survival rate reported in all screened studies was over 90%, including eight studies in which a 100% survival rate was reported. In 22 studies, the reported survival rate ranged from 95% to 99.9%. Failure was reported most often in short SDIs (less than or equal 13 mm) (n = 88) compared to longer ones (more than 13 mm).
Conclusion:
Survival rates reported for SDI are SIMILAR to those reported for STANDARD width implants.
These survival rates did not appear to differ between studies that used flapless and flap reflection techniques. The failure rate appeared to be higher in shorter SDIs than in longer ones in the studies in which the length of the failed implants was reported.
SDIs could be considered for use with FIXED fixed restorations and mandibular overdentures, since their SUCCESS RATE appears to be COMPARABLE to that of regular diameter implants. They might also be an efficient, low-cost solution for elders who wish to reduce problems with denture instability.
2: MDI ClinicalStudies from AroundTheUSA
Willimantic ,Connecticut 2015
Mini Implants Supporting Fixed Partial Dentures in the Posterior Mandible: A Retrospective (2015)
Dennis Flanagan, DDS, MSc
Journal of Oral Implantology e138 Vol. XLI/No. Four/2015
http://www.joionline.org/doi/pdf/10.1563/
AAID-JOI-D-14-
00081?code=aaid-premdev
Small-diameter, or mini dental implants have been successfully used to support removable and FIXED oral prostheses.
These implants impart about twice the per-square-millimeter force on the supporting bone and this should be addressed during treatment planning. In the posterior jaws, bite forces are of a higher magnitude than in the anterior jaws and may induce an overload of the supporting bone and failure of the osseointegration.
Thus there should not be occlusal contact in functional excursions that induce off axial loads.
The cases presented herein demonstrate that mini dental implants may be used successfully to support fixed partial dentures in mandibular sites in highly selected patients.
Mini or small-diameter dental implants (,3.2 mm) have been used successfully for many years.1,2
Probably most of these have been used to retain removable partial and complete dentures.
Nevertheless, many clinicians use mini implants to support fixed complete and partial dentures.
There have been no long-term randomized blinded controlled trials of this treatment or a failure rate established.
Many patients have site conditions, or medical or psychological conditions that preclude the use of standard-diameter implants (3.25 mm).
These patients may not be able to undergo augmentation procedures or they may object to a larger metallic foreign body being placed in the jaw.
Economics may be an issue as well.
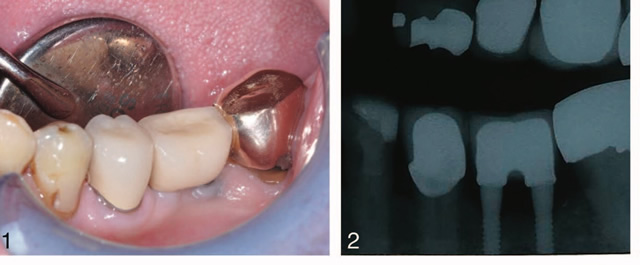
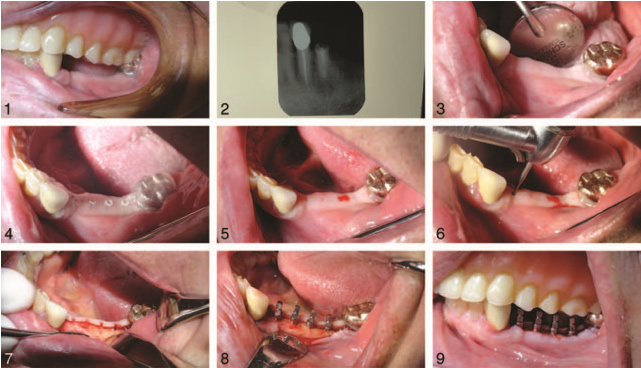
FIGURE 1. The crowns and fixed partial dentures were fabricated with a very narrow occlusal table to minimize off-axial loads.
FIGURE 2. A recent radiograph demonstrates little or no bone loss. No graduated operative radiographs were made so bone loss measurements could not be made.
Mini implants may be placed in many of these patients without substantial augmentation procedures and surgical trauma may be much less.
In addition, the cost of mini implant surgery is substantially less than standard diameter implants.
Some clinicians may feel comfortable using mini implants to support fixed partial dentures in the posterior mandible.
The posterior mandible has a higher occlusal load magnitude with multidirectional cyclic loading. This subjects the bone-implant- prosthesis complex to more severe loading conditions than in anterior sites. This may affect the longevity of the treatment outcome so treatment planning for this parameter is of paramount importance.
The object of this effort is to demonstrate that in highly selected cases with appropriate prosthetic design and osseous support, mini implants may be successfully used to support fixed partial dentures in the mandible.
All patients had medical, economic, psychological, and or attenuated site reasons that made standard diameter implants not an option for treatment.
All implants were small diameter ranging from 2.0-3.0 mm manufactured by Imtec (Irvine, Calif), IntraLock (Boca Raton, Fla), or Biohorizons (Birmingham, Ala).
All prosthetics were single crowns, 2, 3, or 4 splinted prosthetic units fabricated in porcelain fused to noble alloy (PFM) by a commercial dental laboratory (York Dental Lab, Branford, Conn).
All implants were placed in healed, partially edentulous sites. Prosthetic design included a very narrow, rounded, occlusal table, less than premolar dimensions, with absolutely no occlusal contact in functional excursions (Figures 1 and 2). Esthetic compromises were accepted preoperatively by all patients.
All prostheses were made with a flat narrow rounded occlusal table with little artistic anatomical recreation by the technician.
The laboratory technician was instructed to place 3 coats of die separator to ensure a passive fit and account for the expansion.
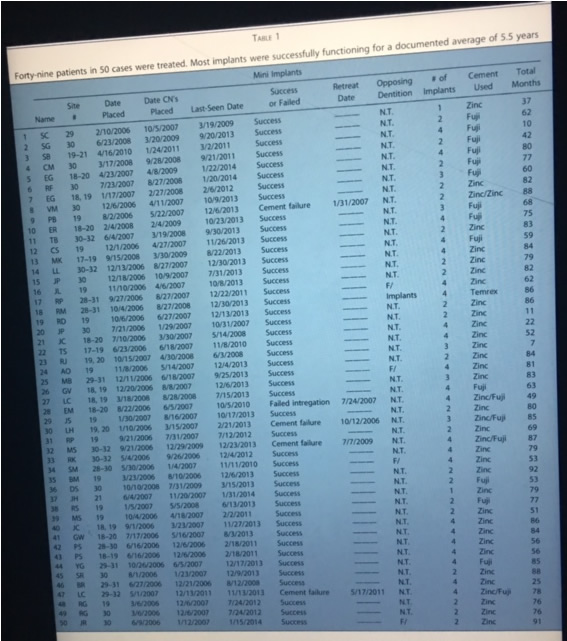
TABLE 1
Forty-nine patients in 50 cases were treated. Most implants were successfully functioning for a documented average of 5.5 years
FIGURE 1. The crowns and fixed partial dentures were fabricated with a very narrow occlusal table to minimize off-axial loads.
FIGURE 2. A recent radiograph demonstrates little or no bone loss.
recemented with insoluble resin modified glass ionomer cement (FujiCEM, 3M
The percutaneous portion of mini implants is much LESS than standard sized implants and thus presents less of an opportunity for coronal epithelial attachment issues.
The circumference (pi 3 diameter) of a 2.5-mm mini implant is 7.85 mm as compared to a standard-sized implant (4.0 mm) at 12.56 mm, which is 160% longer.
This presents much LESS of an opportunity for PERI-IMPLANTITIS, but the rate of peri-implantitis in mini implants has not yet been reported.
CONCLUSIONS
- These cases demonstrate that many patients with conditions that may preclude standard diameter implant treatment, may be treated with mini implant-supported FIXED partial dentures. This is a highly selective and exclusive group of patients that may qualify for such treatment.
- Particular care should be given to bone density of the site, observation of a 4-month healing time, flapless placement, use of longer implants than 10 mm, treatment of any existing periodontitis, choice of an insoluble luting cement, exclusion of occlusal contact in excursions, and very slow seating rotation with intermissions and water irrigation during seating.
- As a retrospective case series this work is a lower level of credibility. More study of occlusal design, materials, and bone resistance physiology is needed to develop this treatment concept.
3: MDI ClinicalStudies from AroundTheUSA
Willimantic ,Connecticut 2008
IMMEDIATE PLACEMENT OF MULTIPLE MINI DENTAL IMPLANTS INTO FRESH EXTRACTION SITES: A CASE REPORT 2008
Dennis Flanagan, DDS
Journal of Oral Implantology Vol. XXXIV/No. Two/2008
http://www.joionline.org/doi/pdf/
10.1563/1548-1336%28
2008%2934
%5B107%3AIPOMMD%5D2.0.CO%3B2
This case report discusses the immediate placement of 3 mini dental implants into 3 fresh extraction sockets. The implants were used to support a SPLINTED FIXED PARTIAL DENTURE.
Immediately placing implants of a very small diameter into fresh extraction sockets to support a FIXED PARTIAL DENTURE is possible.
Some implant sites cannot accept standard-sized implants because of length or width deficiencies.
Very small diameter implants may be able to support FIXED prostheses in these sites.
Immediate placement of implants into fresh extraction sockets may preserve bone and speed treatment.
CONCLUSIONS
Immediate placement of multiple mini dental implants into fresh extraction sockets can support a medium- span FIXED partial denture.
4: MDI ClinicalStudies from AroundTheUSA
Willimantic ,Connecticut 2011
The Mini Dental Implant in Fixed and Removable Prosthetics: A Review : A REVIEW 2011
Dennis Flanagan, DDS1* Andrea Mascolo, DDS2
Journal of Oral Implantology Vol. XXXVII/Special Issue
http://www.joionline.org/doi/pdf/
10.1563/AAID-JOI-
D-10-00052.1
Mini implants may be IMMEDIATELY LOADED in the appropriate osseous situations and may provide an alternative treatment if OSSEOUS CONDITIONS preclude a standard sized implant approach.2,3,11–14
In situations where there is an INADEQUATE INTERDENTAL SPACE, REDUCED INTEROCCLUSAL SPACE ,convergent adjacent tooth roots or close proximity of adjacent tooth roots or narrow atrophic osseous contour, mini implants may be appropriate.1–
Mini implants are consistent with the trend towards MINIMALLY INVASIVE DENTISTRY. Minimally invasive dentistry has been brought to the forefront by some practitioners and may be applied to implant dentistry where appropriate.
FIXED PROSTHETICS
The esthetic zone is wherever the patient deems it to be.
Patient expectations may be unrealistic and acceptance of potentially smaller prosthetic coronas may be objectionable to certain patients.
TWO mini implants may be used for certain mandibular tooth-bound MOLAR SITES to accept a splinted crown restoration.3,22
GENERALLY, these sites have shortened site lengths where a standard diameter implant may not fit with adequate tooth-to-implant spacing.
TWO (2) mini implants can resist axial forces.
However, rounded and narrow prosthetic teeth may be required to present a small occlusal table to minimize off-axial forces.2,3
Single mini implants may support single crown restorations (Figures 7 and 8). Sites with short interdental space (less than 5 mm), such as maxillary lateral and mandibular incisors, and sites where tooth movement has imposed on the site length or the local anatomy is diminutive may accept a single mini implant.3,23 Anterior sites may be more appropriate because of lower occlusal forces.
When mini implants are SPLINTED in FIXED partial or complete dentures, the adjacent implants are ANCHORED to each other, DISSIPATING FORCE and MINIMIZING the potential for implant MICROMOVEMENT .
However, cement loosening in one abutment may cause the fixed bridge to rotate slightly on the cemented abutment and lose osseointegration. An astute clinician may choose to definitively cement only mini-implant–supported prostheses to prevent this complication.
The most retentive metal-to-metal cements are the RESINS and resin-modified glass ionomers.
CONCLUSIONS
MINI DENTAL IMPLANTS may be appropriate to retain removable prostheses and support FIXED complete and partial dentures.
Following are suggested initial GUIDELINES for MINI IMPLANT USE:
Type I and II (Misch) bone sites are most appropriate for mini implants
Minimum of 1-mm thickness of facial and lingual cortical bone
Approximately 100 mm occlusal relief for fixed prosthetics A rounded minimal occlusal table
Minimum space of 0.5 mm between tooth and mini implant
Minimum of 6 mini implants for removable complete dentures in the maxilla
Minimum of 4 mini implants for removable complete dentures in the mandible
Minimum of 10 mini implants for SPLINTED FIXED complete prosthetics in the MAXILLA
Minimum of 8 mini implants for SPLINTED FIXED complete prosthetics in the MANDIBLE.
Implant protective type of occlusal scheme for fixed Prosthetics.
Esthetic requirements are addressed preoperatively
Polyurethane working die material or material of similar durability
EXTRA DYE SEPARATOR may be indicated
Most of the mini-implant evidence is based on retrospective data, case series, or uncontrolled studies. Randomized, controlled, prospective, longitudinal human trials are needed to further validate this treatment.
5: MDI ClinicalStudies from AroundTheUSA
Willimantic,Connecticut 2006
IMPLANT-SUPPORTED FIXED PROSTHETIC TREATMENT USING VERY SMALL-DIAMETER IMPLANTS: A CASE REPORT 2006
Dennis Flanagan, DDS, is in private practice in general dentistry. Address correspondence to Dr Flanagan at 1671 West Main Street, Willimantic, CT 06226 (e-mail: dffdds@charter.net).
Journal of Oral Implantology 34 Vol. XXXII/No. One/2006
http://www.joionline.org/doi/
pdf/10.1563/778.1
Patients present for implant treatment with variable amounts of bone volume, ridge length, and interocclusal space. Some sites are NOT amenable to the standard sizes of many available implants.
Most dental-implant companies offer standard-diameter implants in the range of 3.75 to 4.2 mm, but smaller diameters are available from 2.0 to 3.3mm
Patients present for implant treatment with VARIABLE amounts of bone volume, ridge length, and interocclusal space. Some sites are NOT amenable to the standard sizes of many available implants.
Small-diameter implants have been used for retention of complete maxillary and mandibular overdentures, but there is a dearth of reports for their use in FIXED prosthetics.5 (Mazor Z, Steigmann M, Leshem R, Peleg M. Mini-implants to reconstruct missing teeth in severe ridge deficiency and small interdental space: a 5 year case series. Implant Dent. 2004;13:336–341.)
STANDARD available implants may NOT be appropriate for patients’ compromised sites when the patients present for treatment.
An up-to-date and pervasive knowledge of the ARRAY of implant SIZES and SHAPES is an ASSET for treatment.
Implant diameters are available from 1.8 to 8 mm.
Many implantologists believe that a smaller-diameter implant is MORE DESIRABLE than a LARGER larger one for REASONS of BLOOD SUPPLY ,that is, LARGER -diameter implants may IMPEDE the blood supply to bone surrounding the implant.
Additionally, if an unforeseen bone density or site inadequacy is encountered during the osteotomy of a small-diameter implant, the use of a slightly larger-diameter implant that is able to attain better initial stability remains an option, if there is adequate space.
Consequently, it may be BETTER to have a BIAS TOWARD a smaller-diameter implant rather than one with a larger diameter.
At times, larger- diameter implants may be better suited in the esthetic zone for emergence profile of the crown.
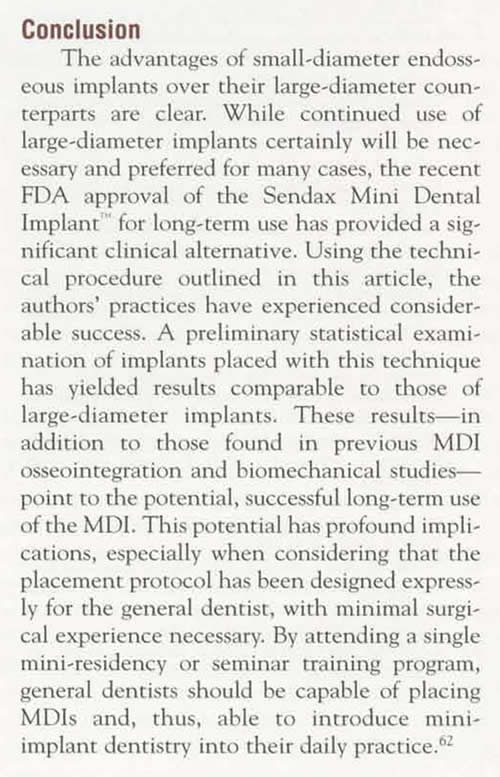
Conclusion:
STANDARD available implants may NOT be appropriate for patients’ compromised sites when the patients present for treatment.
An up-to-date and pervasive knowledge of the ARRAY of implant SIZES and SHAPES is an ASSET for treatment and the implantologist.
Implant diameters are available from 1.8 to 8 mm
The use of very small- or mini-diameter implants may be advantageous.
Sites with inadequate length may be suited for these implants to provide adequate support for the prosthesis.
The AVAILABLE BLOOD SUPPLY around and about a SMALL diameter implant may be BETTER than that of a LARGER -diameter implant.
Sites accepting these small-diameter implants should be of denser bone types I and II.
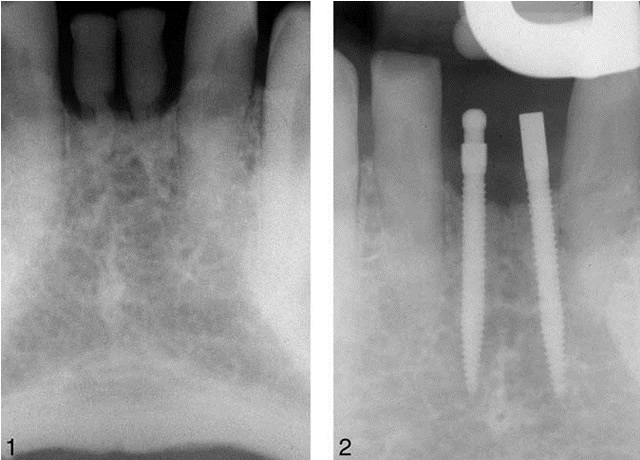
FIGURE 1. Preoperative radiograph. FIGURE 2. Postoperative radiograph of 1.8-mm diameter implants. ,
FIGURE 3. Slightly prepared coronals. FIGURE 4. Cemented prosthesis in place.
6: MDI ClinicalStudies from AroundTheUSA
Willimantic,Connecticut 2008
Fixed Partial Dentures and Crowns Supported by Very Small Diameter Dental Implants in Compromised Sites
Dennis Flanagan, DDS 2008
IMPLANT DENTISTRY / VOLUME 17, NUMBER 2 2008 183
Very small diameter (1.8 –3.3 mm) dental implants may be successfully used to support FIXED partial dentures in edentulous sites of COMPROMIZED bone width or length.
Very small implants can be successfully used in highly selected sites where there is ADEQUATE bone density and bone volume for immediate implant stability.
Adequate or augmentable attached gingiva may be a requirement. A small diameter implant presents less of an obstacle for angiogenesis and there is less percutaneous exposure and bone displacement as compared with standard sized implants. In posterior sites, rounded and narrow prosthetic teeth present small occlusal tables to minimize ax- ial and off-axial directed forces.
MULTIPLE SPLINTED IMPLANTS may be necessary to minimize metal FATIGUE from cyclic loading.
Anterior restorations supported by mini implants may need occlusal relief to minimize the effects of cyclic loading. (Implant Dent 2008;17:182–191)
Key Words: mini implant, occlusal scheme, bone density, bone ridge
There are case reports that demonstrate where compromised sites are re stored with 1.8 to 3.3 mm diameter implants that support FIXED partial denture prostheses.5–7
However, these very SMALL diameter implants, when used individually or in MULTIPLES or in COMBINATION with LARGER sized implants, may offer ADEQUATE support as compared with STANDARD sized implants.
In posterior sites, rounded and narrow prosthetic teeth present SMALL OCCLUSAL TABLES to minimize axial and off-axial directed forces.
Multiple splinted implants may be necessary to minimize metal fatigue from cyclic loading. After trauma or years of bone resorption patients can present for implant treatment with variable amounts of bone volume, length and height of ridge, and interocclusal space. Some sites CANNOT accept the standard sizes of many available implants without site development.
There is some debate as to the true supportive quality of GRAFTED BONE .
Conclusion
Major bone grafting procedures of extremely resorbed mandibles may NOT be justified.
(Int J Oral Maxillofac Implants. 2006 Sep-Oct;21(5):696-710.
The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials.
Esposito M1, Grusovin MG, Coulthard P, Worthington HV.)
CASE SR
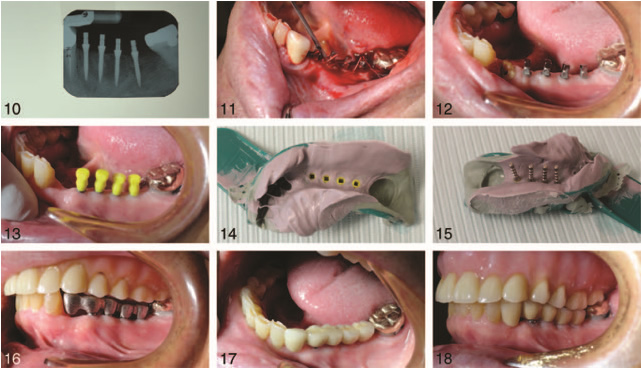
A 61-year-old women had a cari- ous tooth #30 extracted (Figs. 4–6) (Table 1). After 4 months of healing, two 2 1.5 mm implants (Intra Lock, Ultimatics, Ardmore, OK) were placed and restored with a 2 unit por- celain fused to metal crown splint.
CASE VM
A 42-year-old women lost #30 due to failed endodontic therapy (Figs. 7–10) (Table 1). The tooth was sec- tioned and atraumatically extracted and the site allowed to heal for 4 months. Two one-piece 3 mm 12 mm (BioHorizons) were placed flap- lessly by infiltration local anesthesia (articaine). After 4 months waiting for osseointegration, the coronal ends were prepared for splinted crowns. The crowns were cemented with zinc phos- phate cement. The patient has been functioning successfully for 2 years.
CASE JC
A 40-year-old man had lost his mandibular right posterior teeth (Figs. 11–13) (Table 1). The site at #28 was adequate but the edentulous site at #29 –32 was very narrow, precluding implant placement without extra- cortical bone grafting. Four 2 1.5 mm (IntraLock) and a 4 0 mm (3-I) implants were placed and restored with a splinted fixed partial dent
These cases demonstrate that single and multiple very small implants may successfully support crowns or FIXED partial dentures where there is appropriate bone and occlusal considerations.
These sites are usually found in the POSTERIOR mandible and anterior maxilla and mandible.
Because bone volume and quality and ridge length can present the implantologist with a challenge for restorative treatment, creative but effective solutions may need to be considered.
An up-to-date knowledge of the ARRAY of implant sizes and shapes is an asset for treatment.
Bone density of type I, II or III, bone site length of at least 4 mm, bone available height of at least 10 mm and at least 1 mm of attached or augment- able gingiva are desirable. Any in- traoral locat However, LESS dense bone may require the use of LONGER small diameter implants to resist occlusal forces and present less per square millimeter of bone compression during service.
Conversely, there may be PHYSIOLOGIC ADVANTAGE to very small diame- ter implants. An ADVANTAGE that very small diameter implants have over standard diameter implants is the LESSER amount of linear or CIRCUMFERENTIAL PERCUTANEOUS EXPOSURE and BONE DISPLACEMENT.
The circumference of a 2 mm implant is ( diameter) 6.28 mm whereas the circumference of a standard 4.0 mm diameter implant is 12.56 mm.
The very small implant has HALF of the linear percutaneous exposure thus exposing LESS of the implant- gingival attachment to BACTERIAL ATTACK.
There is also a smaller silhouette of the very small diameter implant that may present a BARRIER to ANGIOGENESIS and OSTEOGENESIS .
Because dental implants are cylinders or near-cylinders, a mathematic calculation of the outline form or the silhouette area, of a 2 x 10 mm implant may be compared with a 4 x 10 mm implant. Where the area is diameter (width) height. So, 2 x 10 mm 20mm2 and4 x 10mm 40 .
The 2 mm diameter implant presents a barrier to the osseous physiology that is half that of the 4 mm diameter implant. With respect to volume of the cylinder, where volume ( 3.14) (radius squared) (cylinder height), then3.14 square mm 10mm 31.4 mm3 and, 3.14 square mm 10 mm 125.6 cm3.
So to compare these volumes: 125.6/31.4 4.
The 4 mm diameter implant has 4 times the osseous displacement as compared with the 2 mm diameter implant. This difference may be im- portant. Intuitively, this may be a physiologic advantage for the very small diameter implant in that there may be more of an available osseous blood supply for the implant support- ing bone or less of a barrier. In larger diameter implants this larger barrier to blood supply or angiogenesis may contribute to the classic “resorption to the first thread” in the larger implant. The larger barrier may hinder angio- genesis and subsequent osteogenesis around a newly placed implant. Blood supply at the osseous crest may be hindered
With respect to VOLUME of the CYLINDER , where volume = 3.14 x radius squared x cylinder height then3.14 squaremm 10mm 31.4 mm3 and, 3.14 square mm 10 mm 125.6 cm3.
So to compare these volumes: 125.6/31.4 =4
The 4 mm diameter implant has 4 times the OSSEOUS DISPLACEMENT as compared with the 2 mm diameter implant.
This difference may be important.
Intuitively, this may be a PHYSIOLOGIC ADVANTAGE for the very small diameter implant in that there may be MORE of an available OSSEOUS BLOOD SUPPLY for the implant supporting bone or less of a barrier. In larger diameter implants this larger barrier to blood supply or angiogenesis may contribute to the classic “resorption to the first thread” in the larger implant. The larger barrier may hinder ANGIOGENESIS and subsequent OSTEOGENESIS around a newly placed implant. BLOOD SUPPLY at the osseous crest may be HINDERED by the larger implant and produce the characteristic resorption to the first thread. This phenomenon does not seem to be prevalent with the 2 mm diameter implants. Figure 15 shows 3 implants
This CREST BONE RESORPTION phenomenon does not occur in submerged implants but only after second stage uncovery and placement of an abutment. With the very small 2 mm diameter implants this does NOT seem to be prevalent. This may be the result of the smaller diameter and/or the lack of an abutment with a MICROGAP.
The available bone for an implant site in many cases can leave much to be desired. In these cases, the occlusion, a REDUCED VERTICAL DIMENSION and ridge length can present a dimensional problem for space. Very small diameter implants can fit into many of these atrophic sites with adequate interimplant and interocclusal spacing. Esthetics may be a problem in certain sites and caution is advised here.
These very small diameter implants CAN FIT into sites that CANNOT accept standard diameter implants without augmentation. The implants in these case series were generally placed flaplessly or with a split thickness apically positioned flaps thus retaining the periosteum and its blood supply and retaining or increasing the attached gingiva. The bone in these atrophic sites is typically type I or II and well suited for initial implant stability.
Very small diameter implants have been used for many years in completely edentulous cases to retain overdentures without bone grafting. Extracortical bone augmentation grafting may delay implant placement and the resulting grafted bone may not be truly supportive for the implant for many months or years or possibly never.
The BONE at the CREST of the THIN ATROPHIC RIDGE may be DENSE CORTICAL BONE ,which can be VERY SUPPORTIVE for Implants. Posterior sites in the mandible, not in the esthetic zone, may be appropriate for very small diameter implants that support a fixed partial denture.
The FORCES in the POSTERIOR JAWS can be greater than 1000 N of force but this magnitude is in the axial direction of the implant.8 The off-axial vector directive of these forces is much less. The cyclic loading that characterizes human occlusion may induce metal fatigue in very small diameter implants.
Very small diameter implants may need to be used in MULTIPLES to preclude cyclic loading metal fatigue and implant fracture in the posterior mandible9 (Figs. 7, 11).
Unpublished proprietary company (Intralock) data and unpublished data from the author suggests that single 2 mm diameter implants can withstand cyclic direct horizontal coronal loads of 200 N of more than a million cycles. This force represents the maximum force in the anterior jaws that may be humanly generated in the vertical or occluso-apical direction but this force was applied directly horizontally or facio-lingually for the test.
In anterior sites that have adequate width but inadequate length, a very small implant may be appropriate for a single Implant.
In anterior sites that have adequate width but inadequate length, a very small implant may be appropriate for a single implant.5,10 The forces in the anterior jaws can be about a third of the posterior forces, 50 to 200 N. These forces in occlusion, however, are delivered not axially but off axi- ally, a vulnerable direction for the im- plant. This may require more dense bone to resist the higher per square millimeter force placed on the bone by the smaller diameter implant body. Denser bone may preclude micro- movement of the implant and failure of the implant by fibrous replacement. The crowns in these cases may be best left slightly or somewhat out of occlusal contact in centric position and all excursions.
Very small implants may be used in conjunction with standard diameter (3.75– 4.1 mm) implants to support a FIXED prosthesis where there is an area of thin bone next to or near an area that will accept a standard diameter implant.
The cost of very small diameter implants can about 20% to 50% less than standard diameter implants mak- ing treatment less expensive.
If during the osteotomy of a small diameter implant there is an unfore- seen bone density or site inadequacy, the use of a slightly larger diameter implant that is able to attain better initial stability remains an option, given adequate space and density or bone manipulation techniques such as ridge expansion or splitting. Consequently, it may be better to have a bias to placement of smaller diameter than larger diameter implants.
Larger diameter implants may be better suited in the esthetic zone to provide for the emergence profile of the crown. However, in anterior compromised sites, especially where there has been site length attenuation, smaller diameter implants may be appropriate when the occlusal forces can be minimized or eliminated.
When placing very small implants, it is the experience of this author that placement torque should not exceed 50 Ncm. Over compression of the bone may lead to osseous compression necrosis and the implant may fail to integrate. Additionally, higher torque forces may cause fracture of the implant shaft.
Tarnow et al13 determined that there is a 1.4 mm CIRCUMFERENTIAL BONE CREST RESORPTION about implants. This may mean that the appropriate implant site width is the diameter of the proposed implant plus the 1.4 mm cir- cumferential bone resorption at each perspective. Thus, a 4.0 mm diameter implant would require: 4.0 mm 1.4 mm (facially) on 1.4 mm (lingually) 6.8 mm bone width. Very small 2 mm diameter implants do NOT seem to demonstrate this phenomenon. Because of this information smaller diameter implants may be MORE APPROPRIATE for many COMPROMISED SITES.
Knowledge of the available ARRAY of IMPLANT SIZES is an asset for the implantologist. Sites accepting these small diameter implants in this case series were perceived to be of denser bone types I, II and III.
There will be an increased per square millimeter force exerted on the supporting bone by the implants during function. So, MULTIPLE implants may be necessary to dissipate forces among the implants to minimize osseous stress.
POSTERIOR PROSTHETIC TEETH were made in these cases with rounded cusps and NARROW OCCLUSAL TABLES that present a small area for functional occlusal impact and to minimize off- axial forces.
Zinc phosphate cement (Flecks) was used to lute all cases listed but resin modified glass ionomer or resin cement can also be used. Because these implants are not used with conventional osteotomy
Patients who present with a complete maxillary denture with remaining only mandibular anterior teeth may benefit from this modality.
These patients usually have thin atrophic posterior residual ridges that will not accept a standard diameter implant WITHOUT OSSEOUS GRAFTING.
Because the forces generated by these complete denture patients is generally less than with natural dentition, very small diameter implants may very successfully support FIXED posterior splinted partial dentures.
This treatment may prevent these patients from developing combination syndrome, where there is supereruption of the remaining anterior teeth, fibrous replacement of the ante- rior maxilla and continued atrophy of the posterior edentulous ridges.
Because these implants are NOT used with conventional osteotomy drills but with very thin drills. If the thin ridge is split and expanded with a #15 scalpel the appropriate bone width for a proposed site may be the sum of postoperative peri-implant bone crest resorption of 1.4 mm at facial and lingual, or 2.8 mm. However, there may not be as much resorption as a standard sized implant and the osseous resorption of 1.4 mm seems to not apply to mini implants. This type of osseous crest resorption may not be prevalent with these implants possibly because of less impedance of the blood supply.
So a very narrower ridge may successfully accommodate the mini implant.
7: MDI ClinicalStudies from AroundTheUSA
Willimantic,Connecticut 2016
Case for Smaller Diameter Implants 2016
Dr. Dennis Flannigan
Journal of Oral Implantology : 10.1563/aaid-joi-D-16-00106
http://www.joionline.org/doi/pdf/
10.1563/aaid-joi-D-16-00106
Dear Editor,
Previous work in the dental literature has discussed occlusal over load of dental implants in function.1 Thus larger diameter implants have been advocated.1
However, there are other considerations that may come into play that effect the longevity of an implant. The major parameters are DISPLACEMENT of the IMPLANT, OCCLUSAL OVERLOAD, and PERCUTANEOUS CIRCUMFERENCE.
It may be that the actual larger displacement of LARGE diameter implants IMPEDES BONE REMODELING , especially at the crest where the bone may be thinner at the facial and lingual as compared with the deep medullary bone.2,4
Even if the crestal bone is greater than 1.8 mm the larger implant may prevent adequate angiogenesis for bone remodeling.3,5 Blood supply is important for remodeling. Large diameter implants generally have higher removal torque at initial placement and better stability than smaller diameter implants.1
However, the large physical displacement of wide diameter implants may impede bone remodeling. There may be resorption but not apposition.2 There may be a physical barrier for the blood supply that would inhibit apposition but allow resorption to occur.2,6–8
Assuming, for the sake of simplicity, a length of 10 mm and the implant is a cylinder, the volume of a 5.7 mm implant is 255.047 cubic mm. The volume of a 2.5 mm 3 10 mm implant, again assuming a cylinder, is 49.06 cubic mm. This larger volume may physically impede blood supply and thus impede activity of osteoclasts and osteoblasts thereby impeding remodeling, which in turn may make the cervical supporting bone and epithelial attachment susceptible to peri-implantitis.
Occlusal overload is not generally an issue with large diameter implants due to the large surface area. Dental implants are capable of resisting an axial load beyond human capability. Off-axial loads, however, may not be adequately resisted by the facial or lingual cortices depending on bone quality and volume. A large diameter implant spreads any off axial loads over a larger area than small diameter thus lowering the per square millimeter load on the supporting bone.3
Mini implants, ,3.0 mm in diameter, may demonstrate little or no bone loss over many years of service.9
Nonetheless there is a larger per-square-millimeter load on the supporting bone.
Thus control of the off-axial occlusal load is KEY..
Nonetheless, the small surface area puts a larger per-square-millimeter load on the bone.
This necessitates more dense bone or MULTIPLE SPLINTED IMPLANTS to LESSEN the risk for overload on the supporting bone.6–8
Percutaneous circumference may put LARGER diameter implants at risk for PERI-IMPLANTITIS .2,4
Large diameter implants have a much larger percutaneous circumference as compared with small diameter implants. The small diameter/circumfer- ence may lessen the risk for late peri-implantitis. At least 1 study suggested that larger diameter implants may be more prone to peri-implantitis.5 The percutaneous circumference of a 5.7 mm implant is 15.7 mm whereas that of a 2.5 mm diameter implant is 7.85 mm, which is a dramatic difference. The smaller circumference presents less of an opportunity for invasive bacteria and less risk for any epithelial detachment and infection. 6–8
CONCLUSIONS
Impeded remodeling and increased percutaneous exposure may increase the risk for peri-implantitis in large diameter implants. There may be less risk for peri-implantitis with small diameter implants. Large diameter implant fixtures could be more prone to late peri-implantitis. Long-term randomized controlled studies are needed to elucidate this issue. It may be appropriate to only place implants of a diameter to a maximum of 4.7 mm because larger diameters may impede bone remodeling and present a longer percutaneous exposure.
It is NOT known what thickness, volume, or quality of bone is needed to adequately resist a given occlusal load. It may be that small diameter implants may be surprisingly able to survive long-term occlusal loads. Thus, when selecting an implant for a site, it may be better to err on the side of THIN.
Dennis Flanagan, DDS, MSc Willimantic, Conn
8: MDI ClinicalStudies from AroundTheWorld
Padova,Italy Beirut ,Lebanon 2004
Clinical evaluation of small-diameter implants in single-tooth and multiple-implant restorations: a 7-year retrospective study. 2004
Vigolo P1, Givani A, Majzoub Z, Cordioli G.
Int J Oral Maxillofac Implants. 2004 Sep-Oct;19(5):703-9.
Abstract
PURPOSE:
Placement of small-diameter implants often provides a solution to space-related problems in implant restoration. This 7-year retrospective study presents results from 192 small-diameter implants placed in 165 patients from 1992 to 1996.
MATERIALS AND METHODS:
The dental records of each patient were reviewed. The implants, which were either 2.9 mm or 3.25 mm in diameter, were placed by 2 different surgeons. All prosthetic appliances were fabricated by the same prosthodontist. Ninety-four implants supported single-tooth cemented restorations; the remaining 98 implants supported cemented or screw-retained partial prostheses.
RESULTS:
The total implant survival rate was 95.3%. Four implants were lost at second-stage surgery, and 5 more were lost after loading.
DISCUSSION:
SMALL-diameter implants demonstrated a SURVIVAL RATE SIMILAR to those reported in previous studies of STANDARD-size implants.
CONCLUSIONS:
The results suggest that small-diameter implants can be SUCCESSFULLY INCLUDED in implant treatment. They may be PREFERABLE in cases where space is limited.
9: MDI ClinicalStudies from AroundTheUSA
Buffalo, New York 2003
Mini Dental Implants for the General Dentist
A Novel Technical Approach for Small Diameter Implant Placement
Todd Shatkin,DDS, Samuel Shatkin, DDS, MD,
JADA 2003 Vol. 24,No. 11
Compendium / November 2003
10: MDI ClinicalStudies from AroundTheUSA
Buffalo,New York 2007
Mini Dental Implants for Long-Term Fixed and Removable Prosthetics: A Retrospective Analysis of 2514 Implants Placed Over a Five-Year Period
Todd E Shatkin, DDS; Samuel Shatkin, DDS, MD; Benjamin D. Oppenheimer, DDS; Adam J. Oppenheimer, MD 2007 February 2007 Issue – Expires February 28th, 2009
Compendium of Continuing Education in Dentistry
https://cced.cdeworld.com/courses/99
Abstract
Over the past decade, endosseous implants of increasingly smaller diameters have been introduced into the field of dentistry. Small diameter implants (SDIs) are generally 2.75 mm to 3.3 mm in diameter. They are frequently used in cases of limited alveolar anatomy. Mini dental implants (MDIs) are smaller than their SDI counterparts, with diameters ranging from 1.8 mm to 2.4 mm.
They are suitable for long-term use—a task for which the device was approved by the Food and Drug Administration.
The following study describes the authors’ experience with MDIs under this indication. Over a 5-year period, 2514 MDIs were placed in 531 patients. The mean duration of follow-up was 2.9 years.
The implants supported FIXED (1278) and removable prostheses (1236), with nearly equal placement in the mandible and maxilla (1256 and 1258, respectively).
The overall implant survival was 94.2%. Based on a Cox proportional hazards model, statistically significant predictors of failure include use in removable prostheses (hazard ratio = 4.28), the posterior maxilla (3.37), atrophic bone (3.32), and cigarette smokers (2.28). Implant failures (145) were attributed to mobility with or without suppuration (19% vs 81%, respectively). The mean failure time for these implants was approximately 6.4 months (193 ± 42 days). This temporally correlates with the osseointegration period. A learning curve was established for this procedure, and implant survival improved with placement experience.
Based on these results, the authors have devised treatment guidelines for the use of MDIs in long-term FIXED and removable prostheses.
MDIs are not a panacea; however, proper training enables the general dentist to successfully implement MDIs into clinical practice.
– See more at:
https://cced.cdeworld.com/courses/
99#sthash.6VvFKZP5.dpuf
11: MDI ClinicalStudies from AroundTheUSA
Buffalo,New York 2012
Mini Dental Implants: A Retrospective Analysis of 5640 Implants Placed Over a 12-Year Period 2012
Todd Ellis Shatkin, DDS; and Christopher Anthony Petrotto
Compendium , Volume 33,Special Issue 3. September 2012
Abstract:
Mini dental implants are becoming increasingly popular in dental care today. Because of their smaller size they are often used in cases of limited bone anatomy. Mini dental implants have diameters ranging from 1.8 mm to 3 mm and are suitable for long-term use.
This article describes a retrospective analysis of 5640 mini dental implants placed into 1260 patients over a 12-year period. The mean length of follow-up was 3.5 years. The implants placed supported removable (2319) and FIXED prostheses (3321), with placement in the maxilla (3134) and mandible (2506).
The overall implant survival was 92.1%. Failures of implants (445) were attributed to mobility of the implant; the mean time to failure for these implants was 14.4 months. The small size of these implants has led to the development of techniques that enable placement and use in a short amount of time for both the doctor and patient.
The high rates of success show that mini dental implants are suitable for use in supporting FIXED and removable prosthetics.
Using mini dental implants that enable immediate denture stabilization, or single and multiple-tooth replacement in as little as one visit,3 is clearly desirable to patients.
The relatively lower cost of mini dental implants allows for a larger patient-selection base.
Christensen described these implants as simple, predictable, minimally invasive, and relatively inexpensive.4
Additionally, the osseointegration period required for mini dental implants can be significantly shorter than that for conventional implants because of a less aggressive insertion procedure (ie, minimized disruption of the periosteum).
– Because mini implant insertion requires minimal disruption of the periosteum, there is reduced damage to the insertion area.2
Mini dental implants and their function in immediate loading for denture stabilization and FIXED fixed restorations have become increasingly prevalent in the literature.
Implants supporting fixed prostheses were considerably more successful than those supporting removable prostheses, having success rates of 94.7% and 88.4%, respectively.
Further analysis of location of placement revealed a lower mini implant success rate in the maxilla (90.3% anterior; 92.5% posterior) relative to the mandible (92.3% anterior; 94.1% posterior). The reduced implant success rate in the maxilla was likely due to its poorer bone quality relative to the mandible.
Though there exists greater OCCLUSION in the posterior regions of the mouth, higher implant success rates in those areas may be attributed to the use of MULTIPLE implants to support a prosthesis, mimicking the natural root anatomy. Often, TWO(2) implants were used to replace single molars and MULTIPLE implants were used for posterior restorations involving more than one tooth.
Gender also played a role in the survival of implants. Of the 3378 implants placed in females, the overall success was 93.0%, while the success rate of the 2262 implants placed in males was only 90.8%.
Implants were placed in patients aged 13 years old to 95 years old. The distribution of implants by patient’s age is shown in Figure 17. Patients 21 to 30 years of age had the highest rate of success at 95.8%.
There were 445 implant failures observed.
Implants considered as failed presented as being mobile or fractured.
Of those implants that failed, the majority did so in the first 6 months following implantation. Implants not failing in this time following insertion likely attained osseointegration. This correlates with Brånemark’s classical definition of osseointegration of 3 to 6 months in the mandible and 6 to 9 months in the maxilla.21
Conclusion
With the growing demand from patients for fewer office visits, lower cost procedures with immediate results, and shorter recovery time, dental rehabilitation techniques have been developed for minimally invasive, single-stage implant placement. The mini dental implants used in these procedures have been demonstrated to have high success rates. Over a 12-year period, 5640 mini dental implants were placed with an overall survival of 92.1%.
With the proper training,22 consideration for prosthetic subtype, implant location, size, and patient variables, mini dental implants can provide exceptional outcomes. These results are rewarding for the dentist, minimally invasive and affordable to the patient, and have long-term success for both FIXED and removable prosthetics.
12: MDI ClinicalStudies from AroundTheUSA
Buffalo,New York 2017
A Mini Dental Implant Alternative to All-on-Four 2017
Dr Todd Shatkin Brooke Sadkin, and Jared Shatkin
INTRODUCTION
Aesthetic dentistry has evolved throughout the past few decades, specifically in the field of implantology. Patients are preferring endosseous procedures to traditional dentures and other removable prostheses to increase stability and comfort, and to decrease pain.1 Conventional implants require several procedures involving multiple appointments and upwards of a year until completion; although some newer techniques promote a faster completion time. The “All-on-4” technique is an immediate conventional implant procedure in which 4 large-diameter implants (2 in the anterior and 2 in the posterior) are inserted at a 45° angle to take advantage of the available bone and to reduce the need for bone augmentation and/or sinus lift.2 According to Nobel Biocare’s All-on-4 treatment concept manual, a minimum of 5.0 mm in bone width and 8.0 mm in bone height is necessary to begin the procedure.3 (All-On-4 is a registered patent owned by Nobel Biocare developed together with Paulo Malo, DDS, PhD, at the MALO CLINIC.) Though the All-on-4 technique claims to eliminate the need for bone augmentations and sinus lifts, these procedures cannot always be eliminated if the bone quantity does not meet the requirements due to the large diameter of a conventional implant.1-2,4 While the All-on-4 technique offers acceptable support with 4 implants, the endosseous procedure is still invasive and time consuming compared to the immediate and early loading procedures used with mini dental implants. The All-on-4 often requires a minimum of 4 to 6 months before the final restoration is fully completed.4 In addition, if one of the 4 implants fails to integrate or fails following placement of the restoration, the entire restorative procedure must be restarted, additional surgery performed, and the restoration remade. Considering the average fee for All-on-4 is in the range of $30,000 to $40,000 per dental arch, this technique is not affordable for most dental patients.
Technique Using Mini Dental Implants Recently Introduced
Immediate and early loading endosseous procedures with mini dental implants are more desirable to patients in many instances because of the speed of completion, an affordable fee, and it is a less invasive procedure with reduced postoperative discomfort.4 The small size of the mini dental implants (available in several lengths and diameters) eliminates the need for bone augmentation and/or sinus lifts. This is because the mini dental implant can be angled into available bone rather than augmenting the bone.4 The Shatkin Fabricated Implant Restoration and Surgical Technique (F.I.R.S.T.) (patent USPTO No. 7,108,511 B, September 2006; developed by Todd E. Shatkin, DDS) provides for mini dental implant(s) to be placed and restoration(s) cemented in one patient visit.5 The most recent innovation, FIX on SIX (FIX on SIX is a registered trademark owned by Shatkin F.I.R.S.T., developed by Todd E. Shatkin, DDS) offers a combination of the Shatkin F.I.R.S.T. technique using 6 to 8 (or 10) mini dental implants with a 12-unit fixed detachable zirconia full-arch restoration with o-ring implant housings. The restoration is only removed at recall cleanings as the dentist is able to snap off the FIX on SIX restoration. The hygienist will then completely clean the implants, the restoration, and the surrounding tissue and easily reinsert the restoration without patient discomfort. This FIX on SIX procedure is completed in a fraction of the patient’s and the dentist’s time as required by the All-on-4 technique. The success rates of the immediate loading mini dental implant endosseous procedures are competitive with the All-on-4 technique. If one of the mini dental implants were to fail with a FIX on SIX restoration, the failed mini implant can be easily replaced with a new mini implant and o-ring housing placed in the same or different location. In addition, the FIX on SIX restorations are considerably more affordable than the All-on-4 with approximately a 50% to 66% savings. Consequently, the FIX on SIX restorations are more desirable to the patient due to their affordability, greater comfort, reduced treatment time, and the less invasive nature of the procedure.
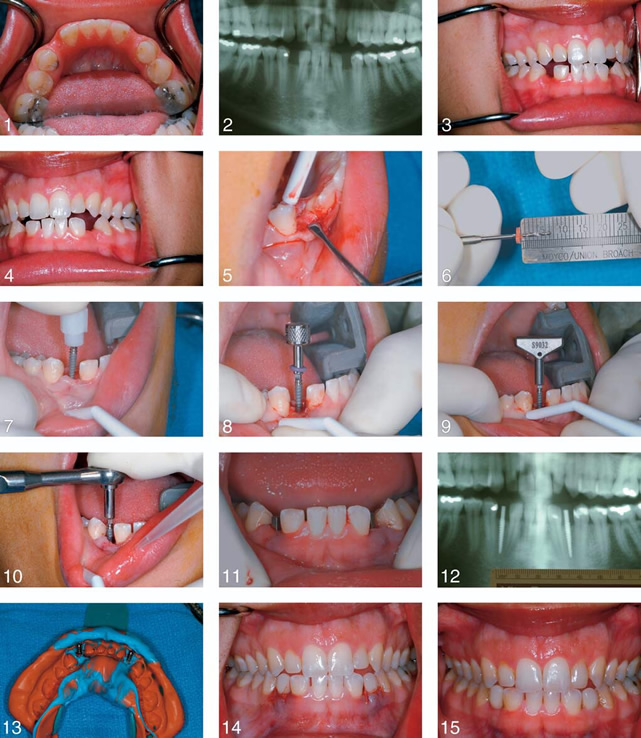
Fixed partial dentures are commonly supported by mini dental implants to provide a natural, aesthetic appearance for the patient. In recent years, zirconium dioxide (zirconia) frameworks have been used in dentistry for fixed restorations.6 The introduction of zirconia has allowed the fabrication of metal-free prostheses via CAD/CAM technology. The result is improved aesthetics with increased success and reliability.7 There is also evidence that there is less plaque accumulation on zirconia, helping to prevent postoperative gingival problems.8 The architecture of these zirconia-based prosthetics enables superior strength and chewing resistance on the posterior teeth relative to other ceramics.5,9 Due to its favorable chemical composition and mechanical properties, clinicians have been eager to use zirconia in implant-supported restorations after its continued success in tooth-supported restorations.10 The following case study (Figures 1 to 15) presents a clinical report of mini dental implants with the FIX on SIX technique. The use of 6 to 8 (or 10) mini dental implants allows for the functional and aesthetically pleasing zirconia fixed prosthesis to be supported. Using CBCT technology, a zirconia prosthetic restoration was created and fixed over Shatkin F.I.R.S.T. mini dental implants (by Intra-Lock) using o-ring housings processed into the zirconia framework.
CASE REPORT
A 56-year-old male patient with an upper denture presented for a consult on May 13, 2016. He had come in after seeing the Shatkin F.I.R.S.T. television marketing campaign. At the consult, our new patient had a CT scan (using our Shatkin F.I.R.S.T. CBCT machine for pre-op and post-op scans) (Figure 1), treatment plan, and impressions taken for a FIX on SIX detachable-removable bridge (Figure 2). To minimize the discomfort and to eliminate the existing issues with his old denture, a zirconia bridge was prescribed and designed to fit on the mini dental implants that would be placed. Zirconia was chosen as the fabrication material due to its strength and durability and resistance to plaque. A treatment plan for placing 10 Mini Drive-Locks (MDL [Intra-Lock]) in the maxillary arch using the Shatkin F.I.R.S.T. technique for mini dental implant placement was chosen. He was asked to return in 2 weeks for his procedure and placement of a temporary bridge.
About one month later, the patient returned, signed the consent form, and treatment was begun. A local anesthetic (2 carpules of Septocaine with epinephrine [Septodont]) was administered. A CT guided stent from Shatkin F.I.R.S.T. Lab was used in this case. The position of the 10 implants was marked using a Thompson marking pen and the CT guided stent (Figure 3). Nine Intra-Lock mini dental implants were used on the upper maxillary arch, size 25 mm/15 mm at Nos. 3 to 6 and 9 to 13; and one 25 mm/11 mm for No. 8. The CT-guided stent was used throughout the procedure (Figure 4), removing it between final placement of each implant, using the patented F.I.R.S.T. technique. When finished placing all 10 implants using the Shatkin F.I.R.S.T. procedure, the housings were placed, and A1 Luxatemp (DMG America) was used to create the temporary bridge. The patient liked the temporary. Impressions were taken and sent to the Shatkin F.I.R.S.T. Lab (Figures 5 to 8). Two prescriptions (penicillin 500 mg, Norco 5/325) were sent to the patient’s pharmacy, and an appointment for 2 weeks was made for the delivery of the permanent FIX on SIX detachable-removable bridge. Two weeks later, the patient returned, and the temporary was removed. The FIX on SIX detachable-removable roundhouse restoration was then placed (Figures 9 to 12). The FIX on SIX restoration had good aesthetics, and the patient was happy (Figure 13 to 15). The patient was given a Shatkin Water Flosser and a Sonicare (Philips Oral Healthcare) toothbrush. These are provided as a part of the treatment to our mini implant patients for optimal home care. These have been very successful hygiene tools to keep the soft tissues healthy and clean between checkups, when the FIX on SIX is removed.
CLOSING COMMENTS
This article presents an alternative to All-on-4 that is less expensive, less invasive and painful, and demonstrates faster results while utilizing zirconia, a strong and biocompatible dental material. FIX on SIX is a beautiful zirconia restoration that can be removed by the clinician while providing the patients with the feel and aesthetics of a fixed prosthesis. Creating a fixed prosthesis that is able to withstand the occlusal forces applied, while providing cosmetic appeal and patient satisfaction, is an enduring task for all dentists.11 Today in dentistry, zirconia has traditionally been used in fixed partial dentures as tooth-supported restorations.9,10 With most cases that use zirconia as a fixed restoration, high success rates have been recorded, mostly higher than 95%.9 Zirconia’s ability to increase the durability of a prosthesis by up to 30% to 40% has made it a good candidate for use in fixed-hybrid cases.11 The use of CT technology increases zirconia’s stability in conjunction with decreasing failure rates of these restorations, due to the industrial processing. In this case study, the patient was dissatisfied with his upper denture because of cracks in the acrylic along the palate, and the dentures were not comfortable to wear, and food would trap under them. By designing a fixed zirconia bridge (FIX on SIX) instead of acrylic dentures or a hybrid acrylic fixed bridge, the patient will no longer have these negative experiences. The use of zirconia instead of acrylic increases durability of the prosthesis while also offering the comfort of fixed restoration and healthier surrounding gingival tissues.
13: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2010
The Truth About SMALL Diameter Implants
Implants Dent Today. 2010 May;29(5):116, 118, 120.
Christensen GJ1, Child PL.
Abstract
SDIs that are treatment planned correctly, placed and loaded properly, and are within a well-adjusted occlusion, are working in an EXCELLENT manner for the patients described in this article.
It is time for those practitioners unfamiliar with SDIs and their uses to discontinue their discouragement of this technique.
SDIs are easily placed, minimally invasive, and a true service to those patients described. They do not replace conventional diameter implants; however, they are a significant and important augmentation to the original root-form implant concept. There is obvious evidence of the growing acceptance of small-diameter implants by both general practitioners and specialists.
If we listened to and believed some of the comments about small-diameter implants (SDIs) (or “mini” implants) that we hear coming from some areas of surgical dentistry, we would be led to think that these devices simply do not work. However,the TRUTH is DIAMETRICALLY opposed to what some are saying, and it has been our observation that some of the most severely negative comments come from dentists who have NEVER PLACED SDIs.
This article includes: the definition of “mini” or SDIs; a discussion of the evolution of SDIs, including their clearance by the US Food and Drug Administration (FDA) and research support; reasons for SDI use instead of conventional diameter implants; the indications for SDI use; and suggestions on how to use them successfully.
The FDA cleared these conventional-diameter root-form implants for clinical use in 1976. Millions of conventional-diameter implants have been placed for more than 4 decades, and their cumulative success rate of around 95% is impressive.
Table. Use of SDIs in Approximate Order of Decreasing Frequency of Use
Edentulous mandible
Removable partial denture
Edentulous maxilla (this use has higher failure rate than edentulous mandibles)
Augmentation of fixed prosthesis
Sole support of FIXED PROSTHESIS
Salvage of previously made prosthesis
SUMMARY AND CONCLUSION
SDIs that are treatment planned correctly, placed and loaded properly, and are within a well-adjusted occlusion, are working in an EXCELLENT manner for the patients described in this article.
It is TIME for those practitioners unfamiliar with SDIs and their uses to DISCONTINUE their DISCOURAGEMENT of this technique.
SDIs are easily placed, MINIMALLY INVASIVE , and a true service to those patients described.
They do not replace conventional diameter implants; however, they are a significant and important AUGMENTATION to the original root-form Implant concept.
There is obvious evidence of the growing acceptance of small-diameter implants by both general practitioners and specialists.
14: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2006
The ‘mini’-implant has arrived 2006
Gordon J. Christensen, DDS, MSD, PhD
http://jada.ada.org March 2006 387 Copyright ©2006 American Dental Association.
JADA, Vol. 137
http://www.smileartsny.com/wp-content/
uploads/download.pdf
What Are Mini- Implants
When the original root-form implants were introduced, they had a diameter of about 3.75 millimeters.
Although I have heard various REASONS for selection of this diameter, the LOGIC for RESEARCH supporting these reasons has been UNCLEAR .
An implant of nearly 4 mm in diameter requires at least 6 mm of bone in a facial-lingual dimension for placement without grafting additional bone to augment the site.
After years of placing implants in all locations of the mouth, it is my observation that SELDOM do I see 6 mm of bone in a facial-lingual dimension.
Often, an osteotome must be used to widen the osteotomy and the minimal bone, thereby allowing placement of the 3.75-mm implant in the less-than-adequately sized bony site.
In the last few years, root- form implants ranging from 1.8 mm to slightly more than 2 mm in diameter have been promoted for long-term service.
IN WHAT SITUATIONS ARE MINI-IMPLANTS INDICATED?
In my opinion, I find MORE indications for narrow-diameter implants (≈ 1.8 mm) than for STANDARD- diameter implants
(≈3.75 mm).
When inadequate bone is present for placement of standard-diameter implants, most practitioners have been taught to suggest bone grafting, either using autogenous bone (from various sites in the patient’s body) or one of the many available bone substi- tutes. However, few patients desire to have, or can afford, bone grafting. The expense of dental implants already is prohibitive for most patients, without the added cost, trauma, pain and uncertainty of bone grafting. In my opinion, if dental implants are ever to achieve their optimum service potential for typical, average-income dental patients, methods need to be found to allow placement of implants in areas of remaining natural bone, using minimally invasive procedures without grafting. The mini-diameter implants have the potential to assist this challenge.
Extra support and retention under fixed partial dentures (FPDs).
Occasionally, situations arise in which an FPD is planned that has questionable potential retention from natural teeth, and the patient has refused RPD treatment or grafting and standard implants. Mini-implants can be placed in the edentulous areas and used to support the PONTIC AREAS of the FPD. When an FPD becomes loose on one end, and the prosthesis can be removed from the other abutment without destroying it, the prosthesis often can be salvaged. A small- diameter implant is placed in the pontic area, a hole is cut in the underside of the pontic, the abutment retainers of the FPD are cleaned and roughened internally, and the FPD is re- cemented using the mini- implant as additional support and retention under the pontic. Research is under way to study the long-term use of small- diameter implants as the full support and retention for fixed partial dentures.
SUMMARY
There is no question that dental implants have been the most influential change in dentistry during the last half-century. In general, they are well-proven and highly useful. However, the diameter of standard implants (≈ 3.75 mm), along with the fre- quent need to graft bone to allow for their placement, have limited their use for those who most need implants. The introduction, approval and continuing observation of success of smaller-diameter mini-implants have stimulated use of implants in situations in which standard- sized implants could not have been used without grafting. The result has been more patients who have been served successfully at reduced cost with minimized pain and trauma patients who could not have been treated with implants otherwise. Continuing research is needed for further verification of the acceptability of mini- implants.
15: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2008
Critical Appraisal MINI IMPLANTS: GOOD OR BAD FOR LONG-TERM ? 2008
Author Gordon J. Christensen, DDS, MSD, PhD* Associate Editor
© 2008, COPYRIGHT THE AUTHORS
JOURNAL COMPILATION © 2008, WILEY PERIODICALS, INC.
DOI 10.1111/j.1708-8240.2008.00204.x VOLUME 20, NUMBER 5, 2008 343
Small-diameter implants combined with natural teeth supporting a fixed prosthesis for 4 years.
In my experience, the majority of patients needing implant support for FIXED or removable prostheses do not have adequate bone present to comfortably place implants 3 mm in diameter and wider without time-consuming, painful, and expensive grafting.
NEED FOR SDIs
The following situations are the most significant clinical indications for SDIs:
1. Inadequate bone present for root-form implants 3 mm in diameter and over
Figure 1 Root-form implants 3 mm and larger in diameter need at least 6 mm of bone in a facial-lingual orientation and 10 mm of bone in a crestal-apical orientation
1. Patient lack of acceptance of grafting for reasons previously stated.
2. Health challenges precluding extensive surgical procedures.
3. Inadequate funds for compre- hensive conventional implant placement and extensive restorative restoration.
I find these indications on a daily basis, and I am thankful that alter- natives other than conventional- diameter (3 mm and over) implants are now available.
My opinion, after using SDIs for over 7 years, is that I have no question about the use of SDIs in appropriate edentulous arches or for augmentation of retention and support for removable partial dentures.
I have had success using SDIs for FIXED fixed partial dentures supported by TEETH and SDIs as well as sole support for fixed partial dentures.
In certain situa- tions, I can support the use of SDIs for sole support of single crowns. Maxillary lateral incisors and lower anterior teeth are excellent examples for single-tooth support.2 My failure rate has been far below that reported in the previous reported survey
My opinion, after using SDIs for over 7 years, is that I have no question about the use of SDIs in appropriate edentulous arches or for augmentation of retention and support for removable partial dentures.
I have had success using SDIs for fixed partial dentures supported by teeth and SDIs as well as sole support for fixed partial dentures.
In certain situa- tions, I can support the use of SDIs for sole support of single crowns. Maxillary lateral incisors and lower anterior teeth are excellent examples for single-tooth support.2 My failure rate has been far below that reported in the previous reported survey.
16: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2008
CRA Foundation Newsletter
Clinician’s Guide to Dental Products & Techniques
Dr. Gordon Christensen
November 2007 Issue 11.
Long term use : Because of the success of minis Minnie as transitional implants & the observed osseointegration, many clinicians began to use them as LONG TERM IMPLANTS.In 1997 Intech miniplant received FDA clearance for Intra bony and intra-radicular …ongoing fixation”,& and in 2003 the “long term intro bony applications”.
Use of minis : Minis were reported most used in edentulous jaws about of both arches & for augmentation of removable partial dentures .
Augmentation of support and retention for fixed partial dentures & support for sole support of single crowns in the areas of minimal bone presence were next ,followed by transitional & orthodontic use.
CRA Conclusions
Currently long-term use of small diameter implant is moving from a relatively experimental mode to MAINSTREAM PRACTICE .Small diameter implants are indicated when patients have minimal bone, denial of grafting ,poor health,minimal financial resources ,and the desire to have minimally invasive surgery accomplished .
Whether or not they will REPLACE conventional diameter implant placement in situations where EITHER COULD BE USED is yet to be determined but is LIKELY TO HAPPEN.
Mini or small diameter implants or minimally invasive, have moderate cost ,are easily accomplished and easily removed if they fail,and have excellent patient acceptance.
17: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2005
The Advantages of Minimally Invasive Dentistry Observations 2005
Dr Gordon Christensen
J Am Dent Assoc,Vol 136,No. 11, 1563-1565
Miniature implants versus standard-size implants
In my opinion, during the past several years, there has been an obvious trend in dentistry toward COMPLEX techniques and accomplishing MORE treatment THAN REQUIRED .
The trend has been mentioned to me many times by colleagues as I have traveled around the world.
Recently ,I had the opportunity to speak at the annual meeting of the World Congress of Minimally Invasive Dentistry. It was refreshing to be with a group of fellow practitioners were attempting to provide OPTIMUM services for patients with the MINIMUM amount of treatment.
OFTEN ,patients do not have the minimum six millimeters of bone in a facial-lingual dimension needed for placement of conventional 4-mm–diameter implants.
The use of “mini” 1.8-mm–diameter implants allows conservative placement of implants in bone that is only 3 mm thick in a facial-lingual dimension, thus avoiding bone grafting and significant trauma and expense for patients.
Placement of these SMALL-diameter implants in MULTIPLES should be considered for optimum resistance and retention of FIXED or removable prostheses.
One widely used brand of mini-implants is IMTEC Sendax MDI (IMTEC, Ardmore, Pa.); another brand is MTI Monorail System (Dentatus, New York). Mini-implants’ minimal cost and ease of placement make them desirable to patients and dentists.2
18: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2008
Christensen ’embarrassed’ by U.S. dentistry DrBicuspid 2008
By Laird Harrison, Senior Editor
https://www.drbicuspid.com/index.aspx
?sec=ser&sub=def&pag=dis&ItemID=301126
October 28, 2008 — The granddad of U.S. dentistry is ashamed of his family.
“What we do in America is embarrassing,” Gordon Christensen, D.D.S., M.S., Ph.D., said at the ADA meeting in San Antonio this month.
With his Clinicians Report review, Scottsdale Center for Dentistry courses, frequent bylines in the Journal of the American Dental Association, and popular talks at dental meetings, Dr. Christensen may be the most influential U.S. dentist. So it means something when he deplores the state of the profession in his own country. Dr. Christensen offered several unfavorable comparisons between dentistry in the U.S. and other countries during a panel discussion about controversies in dentistry, which he moderated at the ADA meeting. He also touched on such questions as mini-implants, cracked teeth, light-activated whitening, and articaine. He mentioned his embarrassment in the context of choosing when a crown is appropriate.
He said many U.S. dentists place porcelain fused to metal (PFM) crowns in cases in which he might recommend an onlay.
“We don’t have to go hog wild with the crowns,” he said. “The typical PFM crown in the U.S. is hideous, absolutely hideous. I go to Switzerland and I have to take my very best stuff because I’m embarrassed by a lot of the stuff we do in America.” The biggest dental organization in the U.S. had no reaction to this criticism. An ADA spokesperson said the association declined to comment. Dr. Christensen did offer a saving grace with regard to U.S. crowns. “We’re doing it at a very moderate level of cost: $800 to $1,000 is the average, where over there you will find $3,000.” But in general, U.S. dentists are losing credibility, he warned. He showed results from a poll in which dentistry had dropped lower in comparison to other professions. “You can see where we are — we’re No. 5. We used to be, believe it not, No. 1. Are we going in the right direction?” Dr. Christensen suggested U.S. dentists have gotten behind on technological trends. When he polled the audience to see how many were using electric handpieces, he noted that, “If I were in London right now or Zurich, all of you would raise your hands.”
Behind on implants
Dr. Christensen also argued that more general dentists in the U.S. should place implants. He estimated that only 6% to 15% of U.S. dentists are placing them now. “I’ve been doing implants for over 20 years,” said Dr. Christensen, who is a prosthodontist. “I find it’s one of the simpler things that I do. There are so many things that are more aggressive and more threatening than doing an implant on a healthy person with good bones…. It’s simpler than doing a third molar extraction.
Yes, you ought to be doing it.”
And once again he said that dentists in other countries are ahead of the U.S. “In Israel, a developing country, 95% are doing dental implants, in Latin America 50% to 60%.”
Dr. Christensen added that dentists should NOT shy away from mini-implants. “Yes, they should be used,” he said. “There are 40 million edentulous people in the United States, and I would guess at least two-thirds or three-quarters of them don’t have enough bone for a normal implant.”
Mini-implants can also save money for frugal patients, he added. “If one of them falls out, big whoopee.
It has expanded the bone, and so when you take it out within even a few weeks, the bone has come back. It’s not like a normal implant with a big hole you need to drain…. Move it over 3 mm and screw in again.”
But technique is important when using these smaller implants.
“They’ve got to be put in right,” Dr. Christensen noted. ”
“Two minis in a surface area of 1.8 mm equals one standard implant, 3.75 [mm].
So put in TWO for ONE and keep them LOW like a sports car, not like an SUV.”
Behind in radiography
Dr. Christensen also argued that “we’re way behind other countries” in adopting digital x-ray equipment. He uses digital himself, in part because of the ease of storing images. But he offered a less than ringing endorsement of the latest high-tech imaging systems, such as standard computed tomography (CT) or cone-beam CT. “You lose the definition, the contrast,” Dr. Christensen said. “You’ve got multiple shades of grey…. Almost every one of those that are digital [radiographs] is second class to an analog radiograph. Period. Exclamation mark. To make them as good, not better, you have to enhance color and texture and go from there.” He said he likes conventional (as opposed to computerized) tomography for planning implants, though periapical radiographs help him “a lot” and panoramic helps “some.” Opinions, opinions
Dr. Christensen also offered his characteristic strong opinions on a wide range of other topics:
• Restoration materials: He pointed to a poll of the American Academy of Esthetic Dentistry. “When asked, esthetic dentists said in their own mouth on second molars, upper molars they want gold. First molars on the lower they want gold. First molars upper they want metal occlusals with porcelain facials. When they got to the premolars and forward, they started talking white.” But in their patients, he said, the same dentists rarely use gold, but instead place white materials all over.
• Light-activated whitening: The lights used don’t get hot enough to make a significant difference, Dr. Christensen said.
• Cracked teeth: There are many types of cracks — superficial cracks in enamel, cracks that extend below the gingival, and cracks that go below the bone. “So here’s my approach: I’ll tell the patient I don’t know where this crack is. I haven’t the slightest idea. I’ll show the patient a video. It shows them these different kinds of cracks,” he said. He then prepares the tooth. A crack that extends below the gingiva but not the bone will fly off during the preparation.
”If it’s down further, slightly under the bone or more under the bone, I don’t know if I can heal it or not. So I’m going to cut the crack and put a provisional on it with Eugenol cement,” Dr. Christensen said. Three or four days later, he asks the patient to bite on a pencil. If the tooth still hurts, he gives the patient a choice between root canal therapy and an extraction.
• Evidence-based medicine: “I get nauseated when I hear this phrase,” he said. Although physician David Sackett, M.D., the father of “evidence-based medicine,” originally incorporated clinical experience into his definition of the phrase, Dr. Christensen complained that too many people in dentistry have forgotten that aspect. “We have got it totally wrong in dentistry right now,” he said. “It’s as if we never had evidence before…. Third parties are using it to our disadvantage.”
• Articaine: U.S. dentists have more problems with paresthesia than European dentists, Dr. Christensen said, because they work too fast and use too large a dose of the anesthetic.
• Bruxism: Dentists should be making more splints, he said. “One-third of the world’s population has aggressive chewing habits. We’re negligent if we don’t say to the patient, ‘You’re chewing your teeth down. Look at mine, I’m 90 years old and mine are long. Look at yours, they’re little bloody nubbins.’ “
What if the patient balks? “A typical bruxing person chews his or her teeth up to six hours a night. A normal person has only a few minutes of tooth contact a day,” Dr. Christensen said. “So I often say, ‘You’re going to have 50 or a 100 days’ wear on your teeth tonight. You need something in there. And if you don’t wear it, you’re going to have teeth looking like this’ — and I show them a picture.”
The session ended at that point, but Dr. Christensen looked ready to offer opinions as long as anyone would listen. If you like this content, please share it with a colleague!
Related Reading
Gordon Christensen on veneers
The inside scoop on which veneers to use and when, plus real-world tips and tools.
ADA Show Report: Gordon C on Perio D
SAN FRANCISCO – In his recent freewheeling talk at the recent ADA convention held in San Francisco, Gordon Christensen paused to ponder periodontal disease…
ADA Show Report: When Gordon talks, dentists listen
SAN FRANCISCO – Gordon Christensen, D.D.S., Ph.D., is no pushover. Dr. Christensen has seemingly used and tested every dental product on the planet.
ADA Show Report: Gordon Christensen: It’s a great time to be a dentist
SAN FRANCISCO – Always informative, always entertaining, always outrageous — that’s Gordon Christensen, D.D.S., Ph.D. Pundit, prognosticator, and pugnacious…
Copyright © 2008 DrBicuspid.com
Last Updated kk 10/31/2008 12:56:57 PM
Forum Comments
9 comments so far …
10/29/2008 2:01:37 PM
Allan Farman
I share Dr. Christensen’s frustrations with the poor quality of dentistry that can be seen in some – or perhaps even many – patients treated in the USA… and also in countries on the other two continents where I hold licenses to practice. What I object to is the misconception that US dentistry is, or has ever been, the torch bearer for dental healthcare internationally. Why should Dr. Christensen be shocked to find excellence in dental care in Switzerland, or for that matter, Sweden, Germany, Italy, Spain, Japan or China? There are excellent training programs in many parts of the world, and in many instances the time spent in training is longer than in the USA and the dental institutions providing the training are extremely well-equipped.
In the USA it is only a recent trend that Dental SCHOOLS have also been viewed as having an important role in dental healthcare for the community. That has happened largely due to state funding drying up and Deans finding that clinical income is often more reliable as an income source than grants and contracts for research. Further, we have essentially reached the limit to the levels to which tuition can be increased given the present state of the economy. Elsewhere, the Dental HOSPITAL has been a center of the highest standards of dental care and a valuable assistance for dental practitioners faced with cases too difficult for them to handle. The equipment comes largely for healthcare rather than for training new dentists alone, and the student dentists get a tremendous exposure to a variety of patient needs and conditions.
So, yes, some dentists in the USA do provide suboptimal care – as do some dentists in most other countries, but nobody should be surprised that excellence in dental care can be found in countries other than the USA.
Allan G. Farman,
Louisville, Kentucky
10/29/2008 6:30:36 PM
powers
This critical observation is right on the point.
Evidence-based medicine: “I get nauseated when I hear this phrase,” he said. Although physician David Sackett, M.D., the father of “evidence-based medicine,” originally incorporated clinical experience into his definition of the phrase, Dr. Christensen complained that too many people in dentistry have forgotten that aspect. “We have got it totally wrong in dentistry right now,” he said. “It’s as if we never had evidence before…. Third parties are using it to our disadvantage.”
10/30/2008 7:40:21 PM
Marty Jablow
Although treatment should not be dictated by insurance companies, in reality it is. So the costs and skill level is greater for inlays/onlays then it is for a crown. Yet, the insurance companies will be pay more for crowns then for inlays/onlays. So we wonder why more crowns are done then inlays or onlays. This is just economic reality for most patients and dentists.
11/6/2008 8:22:46 PM
Hershey
Why is this news? The educational institutions in this country both Public and Private are charging top dollar for inferior education, using information from books that get cover facelifts but not content facelifts. I am a new graduate and I had to relearn dentistry in the past three years using European Texts and Journals. Heck the board exams practice unethical behavior by making practitioners create cavitations in sound teeth that only have radiographic evidence of minor dentin demineralization, how archaic. GV Black techniques are still performed, and this is supposed to be a modern profession? I speak to older dentists and I ask them about the benefits of Glass Ionomers and they look at me with a blank stare! I explain that restorative dentistry for non cavitated lesions is not indicated and could be actually doing harm to the patient and I get angry stares. Yes Insurance companies are dangerous for the single reason that they must show profit growth to Wall Stree every quarter, and of course they like crowns because that allows them to raise premiums which is a dirty way to show positive growth on Wall Street. Dentists love it because they can bang out crowns from China with huge profit margins, everybody is quite happy. Until the patient shows up in 12 months with lots of problems because we failed to treat the underlying disease of pathogenic bacteria. Now we have patients that have lost confidence in this profession because we became salesmen and lost our way of acting like DOCTORS. We need to shape up real fast, start treating the underlying disease and stop thinking that restorative dentistry is a cure for anything, its NOT! Restorative dentistry fills things, replaces things, it DOES NOT CURE antything. There would be no specialty of Endodontics if restorative dentistry cured dental disease remember that fact. We need to place pressure on insurance companies to start reimbursing for PREVENTION AND HYGIENE. Lets give young men and women advice to learn about Dental Hygiene send them to appropriate schools, lets expand our practices to focus on bi-monthly, tri monthly hygiene to actually improve the oral health of our population. Lets push insurance companies to reimburse for Fluoride Varnish treatments. Lets put pressure on the pharmaceutical industry to perfect fluoride and chlorhexidine delivery systems to get our high risk patients under control outside of the office. Lets face it, patients are only in our offices for a few hours per year, we are not really changing their oral health, its what they are doing outside of the office that is changing their health. We need to REFOCUS our way of practicing to meet the future of changing ECONOMICS and DEMOGRAPHICS so that we can regain the confidence of our patients that we actually treat their diseases with long term strategies that are effective. JASON HIRSCH DMD MPH.
11/6/2008 8:42:41 PM
Flatinfifth
I am a new member and I signed up after I read the article on Chistensen’s “embarrasement” with regards to U.S. dentistry as opposed to other countries’ examples of dental care. HOW CAN HE GENERALIZE like that!!!! I am enraged by his comments. It demonstrates a complete lack of understanding of the complexity and multifaceted dilemma facing American dentists in today’s market. He is out of touch. It is 7 PM and I am still at my office finishing up my clinical notes. I began the day at 7 AM. I won’t get home much before 9 and I won’t make it to the gym today. Why?? Because in many American cities unfortunately, insurance companies control the market and we as care givers have to jump through hoops in order to comply. In order for me to “make it” and do what is right for my patients I have to see many patients during the course of a day. And the reason is quite simple; because the fee they “grant” us per service (dictated by the insurance mafia) is extremely low…..an insult in fact. I do end up treating my patients with more difficult and time-consuming restorations (inlays, onlays) even when the fees are lower than for the crown…….because it is the right thing to do. You don’t want to get me rolling in that direction…………..
That kind of statement makes me sick. A terrible way to end my long day. What kind of an embassador do we have representing U.S. dentistry?? Who made him our embassador?? I certainly didn’t vote for him to fill that role…….. Aren’t any of you absolutely disgusted by his posture and pontification?? Isn’t it time that dentists begin to crawl out of their holes and make a stand?? I happen to have lectured abroad as well and I have seen a MUCH LOWER LEVEL of care IN GENERAL in other countries than here in the U.S. Dr. Christensen is dealing with the “elite” of dentistry; those dentists are not the rank and file we find in the trenches. I have seen first hand TERRIBLE examples of dentistry in Europe and Asia……..TERRIBLE; assistants placing composite restorations without bonding, archaic stainless steel crowns sold as permanent restorations, assistants actually preparing teeth and more; why doesn’t he mention that…If I’ve seen it, certainly he must have seen it abroad!!!!!!!! I am sickened by what I see. It’s an outrage…………
Flat
19: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2005
Dental Economics 12-1-05 Ask Dr. Christensen
12/01/2005
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an e-mail to info@pccdental.com.
Question …
I have noticed with interest the growing popularity of the so-called “mini” implants, some of which have diameters about half the size of standard-sized implants. Are these implants successful?
Answer from Dr. Christensen …
I have used mini implants for both provisional and final purposes for several years. In both situations, they have been highly successful. Implant manufacturers report their most popular standard implant diameter is about 3.75 mm. After recognizing the success of these standard-size implants, I was skeptical about the use of narrow-diameter implants that were less than 1.8 mm in diameter. Would they be strong enough? Would they integrate with bone as adequately as the larger implants? Could they be used in both fixed and removable prosthesis situations? Some implant “authorities” condemned the mini implant concept from its inception, which made me even more anxious. Nevertheless, I started using these implants several years ago. Remarkably, the mini implant not only worked, but the technique was far less invasive and easier on me and the patients than the standard root-form implant procedure. I will state my observations of the mini implant concept, and you can make your own conclusions, based on the needs of patients in your practice.
• Amount of bone present. If a potential implant patient does not have approximately 6 mm of bone in a facial-lingual dimension and 10 mm of bone in a crestal-apical dimension, placement of a standard root-form implant is not feasible without grafting. I have successfully placed many mini implants in bone that were only 3 mm wide in a facial-lingual dimension and at least 10 mm wide in a crestal-apical direction. This saves the patient money, trauma, time, and frustration.
• Financial resources of the patient. Today, one typical root-form implant placed in the United States costs a patient about $1,500 without the abutment. The cost of mini implants for practitioners is a fraction of the cost of standard implants. Therefore, most practitioners can afford to place at least two and maybe three mini implants for a fee similar to placing one standard-size implant.
• Invasiveness of the clinical procedure. If adequate bone is present, many mini implants can be placed without reflecting the soft tissue, making a minimally invasive procedure.
• Immediate loading. The manufacturers of mini implants usually suggest immediate implant- loading with which I have had significant success. As an example, patients with poorly retentive removable or complete dentures often eat a normal meal on the day of mini implant placement. They do so with their previously made dentures now stabilized with mini implants. Of course, bone integration still requires several months during which time patients can eat in a normal manner. In summary, do you have patients who have too little bone for standard implants, inadequate financial resources, fear of the typical implant surgery procedure, and the desire to eat easily immediately after implant placement? Of course you do! With proper patient-informed consent about the minimal long-term research on mini implants, and the relatively recent introduction of the mini implant concept, what other choices do you have for many of your patients? Two of our video productions are available for further information. V2300, “Making Decisions About the Successful Use of Implants,” shows the clinical situations in which standard root-form implants can be used; and C900A, “The Mini Implant for General Practitioners,” shows the placement of a mini implant in a simple case.
Question …
When can “mini” implants be used, and when should conventional 3-4 mm diameter implants be used?
Answer from Dr. Christensen …
After several years of using mini implants for long-term service, I have the following observations for your consideration:
➥ Standard size root-form implants are well proven, and in my opinion, should be used whenever possible. When minimal bone is present in a facial-lingual dimension (less than 6 mm), 10 or more millimeters of bone is present in a crestal-apical dimension, and grafting is not feasible, then mini implants should be considered.
➥ As with all procedures, patient-informed consent is mandatory with this concept. Patients should be advised that these implants are being used throughout the world, but they have not been subjected to long-term research such as that done on standard-sized implants. Patients should be informed that, in the event of a failure, removal of the mini implant is simple and replacement is not difficult.
➥ In the event of minimal bone presence – such as 3 or 4 mm in a facial-lingual dimension – reflection of soft tissue is highly desirable to afford optimum vision and adequate mini implant placement.
➥ When using mini implants in situations such as under a complete denture, I suggest that two mini implants should be used where one standard-sized conventional implant would be considered adequate. As an example, four mini implants – two placed in or near each canine area under a complete denture – should be placed instead of two standard implants, one in each canine area. Placement of four mini implants minimizes the possibility of implant rotation as they are integrating into the bone.
➥ As necessary with all implants, patients should be advised to practice excellent oral hygiene. In summary, when adequate bone is not present in a facial-lingual dimension and adequate bone is present in a crestal-apical dimension, and when patients do not want to have bone grafting, then mini implants should be considered. Adequate patient-informed consent should be delivered. Dr. Christensen is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization for dental professionals initiated in 1981. Dr. Christensen is a co-founder (with his wife, Rella) and senior consultant of Clinical Research Associates which, since 1976, has conducted research in all areas of dentistry and publishes its findings to the dental profession in the well-known “CRA Newsletter.” He is an adjunct professor at Brigham Young University and the University of Utah. Dr. Christensen has educational videos and hands-on courses on the above topics available through Practical Clinical Courses. Call (800) 223-6569 or (801) 226-6569.
20: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2009
DentalEconomics11-1-09 Ask Dr. Christensen
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an e–mail to info@pccdental.com.
For more on this topic, go to www.dentaleconomics.com and search using the following key words: small–diameter implants, SDIs, bone–grafting, bone quality, posterior maxilla, anterior mandible, trabecular bone, Dr. Gordon Christensen.
Q I have heard contradictory reports on the success of small–diameter implants, although I have had repeated success using them. The criticisms that I have occasionally heard make me nervous. Should I continue to use them or are there some reservations?
A Thanks for your candid question. I will answer it using research, clinical observations, and my own opinions. I will also make suggestions relative to why a few practitioners have had some failures with small diameter implants (SDIs) or “minis.” You know as well as I do that many patients do not have adequate native bone quantity or quality to place conventional diameter implants, which require at least 6 mm of bone in a facial–lingual dimension, and 10 mm in an occlusal–apical dimension or significant bone grafting. SDIs often can be placed in 3 mm to 4 mm of bone in a facial–lingual dimension and 10 mm in an occlusal–apical dimension. Many patients, especially those in their senior years, cannot tolerate significant surgery, including bone–grafting. They are frequently physically or financially disadvantaged, which further limits their acceptance of conventional diameter implant therapy. SDIs are a proven alternative for many of these patients. As you may know, the FDA clearance for small–diameter implants (<3 mm in diameter) for “long–term use” came in 1997.This FDA clearance came many years after the FDA clearance of conventional diameter (>3 mm in diameter) implants in the late 1970s. Obviously, conventional–diameter implants have proven themselves over decades of use, experimentation, and refinement. In my opinion, root form implants are the most important innovation in dentistry since the air rotor in the late 1950s, and they are now considered a routine part of oral therapy. On the other hand, research on SDIs for long–term use has had only about 12 years to mature. Many innovations in SDIs have taken place during that time, but refinements are still coming, and additional manufacturers are entering the SDI marketplace. As a result, some experienced dentists who have been successfully placing conventional–diameter implants have been skeptical about the long–term effectiveness potential of SDIs. Thus, the active controversy about this subject has continued. Both general dentists and specialists of all varieties are placing implants. There is no specialty for implant placement, although some groups want to claim ownership of this area of dentistry. As an experienced surgically–oriented board–certified prosthodontist, I can say without reservation that a properly educated dentist of any orientation can successfully place root–form implants of any diameter in healthy patients who have adequate bone. I deny the allegations that root–form implant placement is a complex and difficult procedure for dentists who have had proper education and guidance on implant placement. Many other areas of dentistry are more challenging than implant placement. SDIs are certainly no exception. The research on the success of small–diameter implants speaks for itself! Research projects on long–term service of SDIs show more than 90% retention of thousands of SDIs over various periods of time and for a variety of uses. The success percentages rival closely those of conventional–diameter implants. My conclusion on the success of SDIs is that if practitioners are not having success with SDIs, they must be doing something wrong. I will direct the remainder of my answer to that point — i.e., what can you do wrong in diagnosis and treatment–planning, placement, and restoration of SDIs?
Diagnosis and treatment–planning
Bone quality and quantity vary enormously from patient to patient. In case you are not clear on bone classifications, the four classifications (as described by Misch) of oral bone are:
1. D1 — Dense compact, resorbed anterior mandible
2. D2 — Dense to porous compact on the outside and coarse trabecular bone on the inside, anterior and posterior mandible, occasionally anterior maxilla
3. D3 — Thinner porous compact bone on the outside and fine trabecular bone on the inside, anterior and posterior maxilla and posterior mandible
4. D4 — Fine trabecular with little or no cortical bone, posterior maxilla
SDIs range from 1.8 mm to 2.9 mm in diameter. Thus, they are not wide enough to reach dense cortical bone on the facial and lingual surfaces if the facial–lingual bone dimension is wide. Wider–diameter conventional implants are recommended in those areas (4, 5, and 6 mm diameter). The most appropriate locations for SDIs are in dense bone, D1, frequently D2, and D3 when the facial–lingual bone dimension is narrow. D4 is never an appropriate location. If the preceding statements are not recognized and used as guidance for diagnosis and treatment–planning, the SDIs will fail.
Radiographs that show only two–dimensional, panoramic, periapical, or bitewing views do not show the density of bone in a facial–lingual dimension. Tomographic or cone–beam radiographs are strongly recommended before placing any diameter of implant to allow visualization of bone characteristics in a facial–lingual dimension. These types of radiographs are available in most communities if you do not have that capability yourself. If the bone appears to be porous in any dimension, conventional–diameter implants are a better choice than SDIs. Patients having the previously described bone characteristics — i.e., at least 3 or more mm of bone in a facial–lingual dimension and at least 10 mm of bone in an occlusal–apical dimension — are excellent candidates for SDIs (see Fig. 1).
Placement of small-diameter implants
Currently, the most popular SDI brands listed in order of decreasing use are: MDI from Imtec, a 3M Company (Ardmore, Okla.); Atlas by Dentatus (New York, N.Y.), and the ERA Implant System by Sterngold (Attleboro, Mass.). Several other brands are on the market, and others are coming. When adequate bone is present as described, SDIs may be placed without making a surgical flap. However, in my considerable experience placing them, I prefer to make a conservative flap, especially if the bone quality is at all questionable.
The initial osteotomy depth is directly related to the density of the bone. Dense bone requires an osteotomy of up to one–half the length of the implant. Less dense bone should not have deep osteotomies. One–fourth to one–third of the length of the implant is desirable. This allows condensation of the bone as the screw–shaped implant is rotated into place. Making osteotomies too deep dooms the implant to failure. You should feel significant resistance screwing the implant into place for success. As reported by manufacturers, the average length of SDIs placed is about 13 mm. I suggest that shorter implants must be in dense, preferably Type D1, bone for success.
The less the implant protrudes from the bone, the less the lever arm is on the implant when loaded, and the better the chance for success. If coronal soft tissue over the implant is thicker than 2 mm, I suggest removing the excess using a V–shaped wedge on the occlusal and closing it with simple suturing. My recommendations would be to place two SDIs for every location where you might have considered one conventional–diameter implant to be sufficient. As an example, in an edentulous mandible, you may have considered two implants, 3 mm or more in diameter, one in each canine area, to be sufficient.
When using SDIs, two implants either in the general canine area or spread evenly from canine to canine are recommended. Some dentists and companies are using six SDIs in such situations. I have had routine success using four implants in mandibular arches, and occasionally six in the less acceptable bone in maxillas. The implants should be as parallel as possible, although divergence from parallelism up to 15 degrees has been shown to function well.
SDIs are usually loaded immediately on placement, or if a flap has been used, up to two weeks after placement. If waiting to load the implants, make sure that soft denture liner is placed in the old prosthesis to prevent excessive load being placed on the implants during their healing period. The above suggestion reduces or eliminates failure when placing the implants.
Restoration of small-diameter implants
Most dentists using SDIs have experienced success well more than 90% of the time. The uses are listed below in order of decreasing reported frequency of use:
1. Edentulous mandibles
2. Edentulous maxillas
3. Augmentation of retention and support of mandibular removable partial dentures
4. Augmentation of retention and support of maxillary removable partial dentures
5. Augmentation of retention and support of fixed partial dentures
6. Sole retention and support of fixed partial dentures
7. Sole retention and support of single crowns
Categories 1 through 4 have high success, and I do not resist suggesting their use when adequate bone is present. In my opinion, Categories 5 through 7 need additional research and observation. However, many dentists are using SDIs in Categories 5 through 7 with reported success, and I will use SDIs in these situations if there are no other viable alternatives. Restoration of SDIs is no different from restoration of conventional–diameter implants. I have the following suggestions based on my own experience and observation of available research:
• Use flexible “O” ring attachments whenever possible with complete and partial dentures. The flexibility afforded by these attachments reduces the chance of too much load being applied to any implants (see Figs. 2 and 3).
• When the bone is dense, SDIs can use abutments such as the Sterngold ERAs. Four implants in dense bone on the mandibular arch with ERA abutments provide an excellent stable service for patients (see Fig. 4).
• Usually, flexible “O” rings fitting over spheres are used as abutments, but some brands of SDIs, including the IMTEC system shown here, have provided tapered abutments that can be used for fixed prostheses (see Fig. 5.)
In summary, the rumors that SDIs are not acceptable are grossly overstated, and are usually started by persons not familiar with the techniques or research on the subject. If SDIs are planned, placed, and restored properly, there is no reason they should not serve well over many years. To further answer your questions, Practical Clinical Courses has two one–hour videos that show in live, close–up views the placement and restorations of small–diameter implants.
They are:
V2317, “Mini Implants for Your Practice” V2337, “Restoring Mini Implants” We also have a popular two–day, hands–on course offered both in Provo, Utah, and Scottsdale, Ariz., that will further prepare you to place and restore these small–diameter implants. Call or contact PCC for details and dates. For more information, visit us online at www.pccdental.com or contact us by phone at (800) 223–6569.
Editor’s Note: References available upon request. Dr. Christensen is a practicing prosthodontist in Provo, Utah, and dean of the Scottsdale Center for Dentistry. He is the founder and director of Practical Clinical Courses, an international continuing–education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Rella) and senior consultant of CLINICIANS REPORT (formerly Clinical Research Associates), which since 1976 has conducted research in all areas of dentistry.
21: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2011
Dental Economics 11-1-11 Ask Dr. Christensen
Gordon J. Christensen, DDS, MSD, PhD
For more on this topic, go to www.dentaleconomics.com and search using the following key words: small diameter implants, removal partial dentures, Dr. Gordon Christensen.
Q I have been considering incorporating placement of small-diameter implants into my practice, but I hear from some of my surgical friends that there could be failures with small-diameter implants. Are they a viable service, and if so, why are some saying they are not acceptable?
A From the time they were introduced, small-diameter implants (SDIs) have been criticized by some dentists and loved by others. The mini-size implant is usually considered to be up to 2.9 mm in diameter with a typical length of 13 mm (Fig. 1). I am frustrated about why this size of implant has been controversial, and I have some answers for you.
Initially, SDIs were used for transitional support of prostheses, while conventional-diameter implants (3 mm and more in diameter) integrated into bone (Fig. 2). There was no intent to have the SDIs serve for more than the transitional period, and they were taken out as soon as it was considered that the conventional diameter implants had integrated solidly in place.
Initially, SDIs did not have the special sandblasted or etched surfaces that are now known to enhance bone integration and provide long-term service. Similar nonsurface-treated SDIs are currently used in orthodontics as anchors to assist in tooth movement. In the mid-’90s, some dentists began successfully using SDIs for support of complete dentures (Figs. 3 and 4). Pure titanium, the initial composition of SDIs, was soon replaced with titanium alloy, which has greater strength. Etched and/or blasted surfaces began to be placed on the external of the titanium alloy SDIs. The external surfaces on the SDIs were then comparable to conventional-diameter implants.
Imtec, a then-small company in Oklahoma, popularized the use of SDIs during the early and mid-2000s. Imtec is now owned by 3M ESPE and is still the most popular and research-supported brand of SDIs.
SDIs were met with both enthusiasm and ridicule. Those practitioners who took the time to learn to use SDIs found repeated success for numerous indications, but some dentists considered them only transitional in nature, and this impeded the growth and acceptance of SDIs.
It is now over 14 years since the FDA cleared SDIs for “long-term use” (1997). Since then, they have grown in popularity and acceptance. However, with that growth came some improper use of SDIs, and lack of knowledge on the part of some practitioners who started using them without adequate instruction. Undoubtedly, it is primarily those practitioners who have caused the criticism from certain segments of the profession. What are the major indications for SDIs? It is well known among those who place implants that the majority of patients who have missing teeth, especially edentulous patients, do not have adequate bone in a facial-lingual dimension to allow placement of conventional-diameter implants without grafting (about 6 mm of bone facial-lingual is required for conventional-diameter implant placement). Additionally, many patients who have inadequate bone do not want grafting, are too debilitated to have the traumatic surgery required for the grafting, or do not have the financial resources for extensive grafting. The obvious solution for those patients is to use SDIs, which can be placed in a minimum of 3 mm or 4 mm of bone in a facial-lingual dimension. Correctly designed SDIs are gently tapered and screw-shaped with a point on their apical end (Fig. 1), in comparison to conventional-diameter implants, which usually have a blunt end. SDIs spread bone when they are placed, while conventional-diameter implants usually require significant bone removal to allow their placement. Some so-called, but incorrectly designed, SDIs have a point but their taper is far too severe, causing bone fracture, unless significant bone is removed before placement. Inadequate design of some SDI brands is one of the reasons for potential failure.
Because the surface area of the most popular size of SDIs (about 1.8 mm) is about one-half of the surface area of the most popular size of conventional-diameter implants (about 3.75 mm) (Fig. 1), two appropriately spaced SDIs are usually indicated to be placed where one conventional-diameter implant would have been used. I have been successfully placing SDIs for about 11 years. I will share my personal opinions on their indications based on my experience and surveys of practitioners we have accomplished in Clinicians Report Foundation. The following list is ordered from most indicated and successful to least indicated and successful, with some narrative on each:
1) Fully edentulous mandible. This is by far the most significant indication. The bone in this indication is usually dense and strong with minimal trabeculation porosity (Type 1 bone). Usually, four SDIs spaced from canine area to canine area are adequate (Fig. 5). Seldom does failure occur in such locations unless the implant is placed improperly (described later).
2) Fully edentulous maxilla. Bone in this area is not as dense or predictable as in the mandible (Type 3 bone). As a result, more SDIs should probably be placed to ensure success by better sharing of the occlusal load. Although I have had success with four SDIs spaced between the canine areas, placement of six is a safer treatment plan.
3) Removable partial dentures. In my opinion, this indication is far underused. Most conventional removable partial dentures (RPDs) are not highly successful. Many patients do not use their partials on a routine basis. Mesial or distal to remaining teeth in a partially edentulous mouth is almost always a triangle of bone into which either an SDI or a smaller conventional-diameter implant can be placed (Fig. 6). In many cases, placement of SDIs in this remaining triangle of bone, with or without a flap, is highly successful and predictable. Many uses for SDIs are present for removable partial dentures (Figs. 7 and 8).
4) Augmentation of support and retention for fixed-prostheses. Occasionally, there exists a span between potential abutment teeth that is considered to be too long for a conventional fixed-prosthesis, and the remaining facial-lingual bone in the pontic area is too minimal for conventional-diameter implants. Infrequently, placement of SDIs in the pontic area is indicated for additional support and retention of the fixed prosthesis. This is a highly controversial use and is considered to be experimental. The implants and teeth supporting the fixed prosthesis conjointly support the prosthesis, and it is mandatory to cement such prostheses with strong cement, such as resin. Provisional cementation of such prostheses is definitely contraindicated, as natural teeth will intrude as the provisional cement breaks loose.
5) Sole support of a fixed prosthesis. I have done this only a few times. This plan is occasionally indicated in lower anterior partially edentulous areas, where there is minimal bone in a facial-lingual dimension and limited mesial-distal space. When accomplished properly and with adequately supportive bone, there is no reason to be concerned about the potential success of the restoration.
6) Support of a single crown. Although suggested by numerous clinicians and documented by some clinical observational studies, this is the most controversial use of SDIs. There are a few cases in which this use may be indicated, such as for congenitally missing maxillary lateral incisors or for a single missing lower anterior tooth. In such limited cases, I suggest placing the SDI, making a space under a “flipper” to accommodate the SDI abutment, loading the space with soft denture reline material, and allowing a few months of bone integration into the implant before loading it. I know I am conservative, but I prefer success to failure.
Use of SDIs as support and retention for removable complete and partial dentures is safe and predictable when accomplished properly. The other uses described here need additional long-term use and observation for validation, and should be accomplished with caution only when other alternatives are not possible.
To make SDIs successful, I suggest the following:
• Make sure bone quality is adequate. Screwing the mini implant into the bone should require 30 NCm or more of torque on insertion.
• Make sure bone quantity is adequate. The longer the implant the better, to a point. The average and most popular length is about 13 mm.
• Observe occlusion carefully. The approximately one-third of the adult population who have bruxism or clenching are not good candidates for SDIs.
• Do not leave more than 2 mm of soft-tissue coronal to the bone.
• Place the SDI as far into the bone as possible, still leaving space for the abutment.
• Place SDIs parallel to one another. More than 15 degrees of divergence is negative.
• Do not place implants too close together. Leave space for the housings or attachments.
If small-diameter implants are placed observing and accomplishing these characteristics, they will serve very well. It is my candid opinion that SDIs are one of the most useful concepts that have been developed in many years, and that when placed properly, they can serve millions of patients that cannot be served with conventional-diameter implants. Our newest DVD, V2551 “Predictable Removable Partial Dentures” shows small-diameter implants used with removable partial dentures. In my opinion, this is one of the most important potential uses for these small implants. The DVD shows every step to using mini implants under removable partial dentures, thus reducing the use of clasps and improving denture support and retention. Please visit our website at www.pccdental.com or call 800-223-6569 for additional information. Dr. Christensen is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization initiated in 1981 for dental professionals. Dr. Christensen is a cofounder (with his wife, Rella) and senior consultant of CLINICIANS REPORT (formerly Clinical Research Associates), which since 1976 has conducted research in all areas of dentistry.
22: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2007
Dental Economics 1-1-07 Ask Dr. Christensen
In this monthly feature, Dr. Gordon Christensen addresses the most frequently asked questions from Dental Economics® readers. If you would like to submit a question to Dr. Christensen, please send an e-mail to info@pccdental.com.
Q I am interested in small-diameter implants because I have been told that they can be loaded immediately after placement. Is that correct?
A Many patients have inadequate bone present for standard diameter implants and will not accept grafting procedures. A viable alternative, the small diameter implant, is continuing to receive wider use and acceptance.
Small-diameter implants (SDIs), “mini” implants, or narrow-body implants are usually described as being less than 3 mm in diameter. Most of them being used today are about 1.8 to 2.4 mm in diameter. These small-diameter implants have been used for many years as provisional support for prostheses, while standard 4 mm-diameter implants were integrating into the bone. Since the late 1990s, many dentists have been using them for long-term support of both fi xed and removable prostheses. IMTEC Corporation received FDA approval for long-term use of its mini implant in 1999. Several companies are now promoting small-diameter implants for long-term use. If adequate bone is present, many of the mini implants can be placed without making a fl ap. However, in some situations, a flap procedure must be accomplished to allow vision of the bone morphology and adequate placement of the implant.
Yes, these small-diameter implants can be loaded as soon as they are placed. Unlike conventional-diameter, root-form implants that are nearly 4 mm in diameter and require a hole nearly the size of the implant for insertion, the current generation of small-diameter implants are much like a screw for a hardwood board. A small, narrow-diameter osteotomy is made in the bone about one-third to one-half the anticipated depth of the mini implant, and the smalldiameter implant is screwed into the bone. The bone is expanded and widened by the implant as it cuts its way deeper than the original osteotomy site. The result is a very stable small implant immediately on placement.
Clinical success continues to be acknowledged with immediately loaded, small-diameter implants, and research is generally positive concerning this concept.
One of our newest videos, #V2317 “Mini Implants For Your Practice,” shows placing and restoring small-diameter implants for removable and fi xed prostheses. Implementation of this concept into your practice will expand prosthodontic services for your patients. For more information, contact Practical Clinical Courses at (800) 223-6569, or visit www.pccdental.com.
Q I have been told that implants should not be attached with fixed bridges to natural teeth. However, I have made several bridges, attaching natural teeth to implants, without any problems. Should implants be connected to natural teeth?
A The answer to your question is both “yes” and “no.” There is very little research that has been accomplished on this important subject. I will provide my own conclusions for you, based on hundreds of implant-supported fi xed prostheses I have accomplished personally. There is no question that making a fi xed prosthesis and cementing it with provisional cement to an implant and a natural tooth is asking for trouble. I learned this as I had some very expensive failures about 15 years ago. Provisional cement is weak and often breaks loose, allowing the natural tooth to intrude into the bone. I have observed natural teeth intrude up to one-half inch after breaking loose from the abutment crown. This intrusion requires only a few months and usually requires removal of the affected tooth and a new, more extensive restoration. Another technique has also given me signifi cant trouble. Early in the history of root-form implants, some clinicians suggested placing precision attachments or keyways between teeth and implants. This sounded like a logical concept. Again, I have had natural teeth intrude up to one half inch when keyways were placed between implants and natural teeth. The only solution to such a problem is usually extraction of the natural tooth. There are situations where natural teeth and implants need to be connected because of inadequate bone in potential pontic areas, or to avoid placing more implants for financial reasons.
The following technique is successful if carried out exactly as outlined below. For our example, I will assume that one natural tooth is being connected to one implant, with one missing tooth being replaced with a pontic:
• Make a full-crown tooth preparation on the abutment tooth. The preparation should be parallel and as long from the occlusal to the gingival area as possible.
• Place an appropriate abutment on the implant. The abutment should be as parallel as possible with the abutment tooth.
• Make the fixed prosthesis.
• On the cementation appointment, make relatively deep rotary-diamond scratches on the tooth preparation.
• Make sure that the abutment is securely attached to the implant.
• Cement the fi xed prosthesis with strong bonded-resin cement.
• Adjust occlusion carefully, placing heavy occlusal forces on the articulation marking ribbon or paper, and reducing the marked areas to allow equal load on the implant and tooth-supported restoration and the adjacent natural teeth. The implant will not move apically, but the tooth can move slightly apically. Inadequate occlusal adjustment can cause premature failure.
• Expect successful service from the natural tooth/implant-supported fixed prosthesis.
Dr. Christensen is a practicing prosthodontist in Provo, Utah. He is the founder and director of Practical Clinical Courses, an international continuing-education organization for dental professionals initiated in 1981. Dr. Christensen is a co-founder (with his wife, Rella) and senior consultant of Clinical Research Associates which, since 1976, has conducted research in all areas of dentistry and publishes its findings to the dental profession in the well-known”CRA Newsletter.” He is an adjunct professor at Brigham Young University and the University of Utah. Dr. Christensen has educational videos and hands-on courses on the above topics available through Practical Clinical Courses. Call (800) 223-6569 or (801) 226-6569.
23: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 200
Mini Implants: Insight from Dr. Gordon Christensen
Inclusive Magazine: Volume 4, Issue 2
with Gordon J. Christensen, DDS, MSD, Ph.D.
Dr. Gordon Christensen, a pioneer in the field of implantology and a leading proponent of small-diameter, or mini, implants, has shared his knowledge and experience during his visits to the laboratory. The following details his recent insights on the current and future state of mini implants.
Mini implants as a permanent solution
Initially, I was using minis as transitional implants when I had placed conventional implants and just wanted something to hold the denture or the fixed bridge in place while the conventional-diameter implants integrated. I found, after three or four months of waiting for the conventional diameter implants to integrate, that I seldom could take the mini implants out easily. In fact, I had a couple that I practically had to cut out. That was the turning point. When the early transitional implants were introduced, they were pure titanium. They were so weak that you could bend them with your finger. They were not adequate. However, when Dr. Victor Sendax (one of the first proponents of small-diameter implants) got together with the IMTEC Corporation and made them from titanium alloy, they were significantly stronger. The combination of strength and ease of placement, and the fact that they could be loaded immediately, made me change my mind about using small-diameter implants.
Current state of implant placement
My observation is that we are only treating a small fragment of the American population who could benefit from dental implants — it’s abominable. At most, maybe 2 percent of Americans have had an implant. A lot of countries I visit have 10 percent, 15 percent, 18 percent. We are basically at nearly zero. We have aimed at the boutique level, but what about the other 98 percent? What about the rest of the people who make around $55,000 a year, the average American salary for a family? We need to get involved with people who have a typical income.
Implant dentistry is on fire! It’s going to continue to grow and grow. It’s going completely beyond what I expected. But we are only hitting the market with the large-diameter implants. We’re not involved with the other part of the population because of high costs. We are going with the big implants and they only fit in patients with 6 mm of bone facial-lingual. Who has that? Not people at age 50 or 60 or 70. They usually don’t have that much bone. So the obvious change is going from just serving the boutique level to treating typical people. Implant dentistry is on fire! … But we are only hitting the market with the large-diameter implants. We’re not involved with the other part of the population because of high costs.
Why so few dentists are placing implants
I’ve been doing surgical placement of implants for about 25 years. As a prosthodontist, it was a very difficult thing to get into because the surgeons wanted to dominate the area. For many years, they did. Now, we are starting to see general practitioners become more involved. But still, there is frustration on their part. Are they going to hit a tooth? Are they going to hit the sinus? Will they perforate the inferior alveolar canal? And all the other negatives that are pretty obvious to any one of us. Yet, a statistic that I’m going to give you right now is very clearly oriented toward the desirability of general practitioners placing implants. We know that about 69 percent of general dentists will do a third molar impaction. According to our legal experts, that is potentially far more legally threatening and problematic than placing an implant — and I’ll qualify this — in a healthy person with good bone. We did a survey recently of 140 procedures in dentistry to identify the difficulty of each on a scale of 1 to 10, 1 being simple and 10 being extremely difficult. An implant, in a healthy person with good bone, got a rating of 5. And so did a Class II composite. Who does most of the routine surgery in dentistry? The general dentist. Most general dentists will take out a third molar, but less than 10 percent will do an implant in a healthy person with good bone. There is an educational demand there.
Courtesy of Christopher P. Travis, DDS
Advantages of mini implants for patients
The primary benefit of mini implants is for a person who is too debilitated to undergo the surgery necessary for conventional implant placement; the person who does not have the money for a complex case, which very often might be better; or the person who will not accept, or cannot have for health reasons, a major bone graft.
Advantages of mini implants for clinicians
Simplicity. In the November 2007 CRA® Newsletter (now Clinicians Report®), when asked about difficulty of implant placement, respondents reported placement without a flap as “simple” and placement with a flap as “slightly more difficult.” That’s about what we saw as the major advantage to the clinician. I delivered a program at the World Congress of Minimally Invasive Dentistry (WCMID) on about 20 different minimally invasive techniques. Minimal invasiveness is one of the major benefits of small-diameter implants. Another significant advantage is that they can be immediately loaded in bone that is adequate. With Type I bone, there’s no question; I’ve loaded hundreds of them immediately.
Minimal invasiveness is one of the major benefits of small-diameter implants. Another significant advantage is that they can be immediately loaded in bone that is adequate
Conditions that cause mini implants to fail
Improper radiography and lack of thorough treatment planning are often the cause of mini implant failure. I strongly suggest a facial-lingual radiograph for any treatment plan — either a tomograph or a CBCT scan. The quality and quantity of bone, as well as the ideal location of the implant, can be evaluated pre-surgically. Too much soft tissue thickness on the ridge is another issue. If the thickness of the soft tissue is more than 2 mm, the clinician should take a V-wedge out and allow the soft tissue to heal before even considering making any kind of an impression. About 2 mm of soft tissue should be the maximum on the crest. Too few implants placed can also be a major problem. For Type I bone, four mini implants in the anterior region of an edentulous mandible is more than enough. I usually say two small-diameter implants would equal one conventional-diameter implant. Besides diameter, the length of the implant must be considered; 10 mm is very borderline. If you’re going through 2 mm of soft tissue, you really don’t have enough bone-to-implant contact. The average length used by the profession is 13 mm. Regarding lining up the implants — and this is totally empirical — I do not like anything greater than 15 degrees from parallel. Usually, the housings will compensate for that quite nicely. If the divergence is too great, the O-rings will wear more quickly. And poorly adjusted occlusion is a total killer. If clinicians attempt to put minis into a bruxer, they’re kidding themselves
Finding success with mini implants
Making minis succeed means adequate numbers of implants and proper treatment planning. It means parallelism. It also means not having too much soft tissue coronal to the bone. It means adjusting occlusion well after the prosthesis is delivered. And, in the event that the bone is of questionable quality, it means waiting, with a soft denture reline, for several months before loading. However, most of the small-diameter implants I have placed were loaded immediately. But there is a cautionary note, and that is: recognizing what makes them fail. If clinicians respect the several points I’ve mentioned, minis will serve patients well for years. Small-diameter implants are a revolution in implant therapy. This is where the action is! Small-diameter implants will satisfy two-thirds of the population who are not well served by larger diameter implants. When we wake up and recognize that and learn how to use those small-diameter implants, we will have a whole new marketplace in our practices
24: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2007-2009
Gordon J. Christensen CLINICIANS REPORT 2009 CRA Newsletter 2007
Minimally Invasive Dentistry Can Be Win-Win
Dr. Gordon Christensen
October,2009
Gordon and Paul’s Too 10 Conceps,Techniques,and Products
Dr.Gordon Christensen
September,2009
Small Diameter ‘Mini’ Implants-User Status Report
Dr.Gordon Christensen
November,2007
25: MDI ClinicalStudies from AroundTheUSA
Provo,Utah 2009
The Increased Use of Small-Diameter Implants 2009
Gordon J. Christensen, DDS, MSD, PhD*,
Many people in the United States are edentulous. Estimates of the percentage of edentulous people vary, but clinicians agree that every practice has a significant number of people wearing complete dentures. Some of these patients are elderly and physically debilitated. Often, because of their health challenges, they cannot undergo the surgery necessary for simple conventional implant placement. Many do not have adequate funds to pay for comprehensive oral care. Additionally, I have observed when treating many of these patients that most of them do not have adequate bone for placement of conventional-diameter (3 millimeters or larger) root-form dental implants. When I have offered these patients relatively extensive bone-grafting procedures that could provide the necessary bone for placement of conventional-diameter root-form implants, most of them have rejected my proposals. The reasons for their refusal are that they do not want to go through the bone-grafting procedure, they cannot afford grafting or both. Consequently, in my opinion, they are a forsaken and forgotten group, destined to go through the remainder of their lives with inadequate oral function, often poor esthetics and, almost inevitably, low self-esteem.
Standard-diameter implants, 3 mm or larger in diameter, received clearance from the U.S. Food and Drug Administration (FDA) for long-term use in the late 1970s.
Their success is well-known. These implants are placed surgically by some general dentists and prosthodontists, most periodontists and oral surgeons and a few other specialists. When patients are healthy and they have adequate bone, root-form implants larger than 3 mm in diameter provide simple, relatively nontraumatic and highly appreciated treatment. However, many times adequate bone is not present, especially in the areas of severe need for retention and support of fixed or removable oral prostheses. I will outline three prosthodontic methods for restoring only one of the most debilitating clinical situations, edentulous mandibles. I consider this oral condition to be the most severe, and also the most neglected, commonly occurring malady in dentistry. In this treatment, the dentist places four to six SDIs, usually ranging from 1.8 to 2.9 mm in diameter, as parallel to each other as possible and anterior to the mental foramen. Small spheres on the coronal portions of the implants are projections of the implant body extending a few millimeters from the gingival tissues into the oral cavity. A standard mandibular denture impression, made in a custom-fitted tray or in the patient’s existing denture, includes the implants, the residual mandibular ridges and the border-molded oral mucous membranes. The laboratory technician places analogues into the wells made by the implants in the impression and pours the impression in the usual manner. When the impression is separated from the stone cast, the analogues representing the implant abutment heads protrude from the cast. The dentist places metal housings containing rubber O-rings on the analogue heads and processes the denture to retain the housings and O-rings. He or she adjusts the denture in the usual manner, evaluating fit, pressure spots, occlusion and esthetics and then making any necessary corrections. The dentist or dental hygienist will need to replace the rubber O-rings periodically, as they lose their ability to retain the denture in place during service. This concept is the one used most commonly for SDIs in patients with edentulous mandibles (Imtec manufactures a well-known brand).1, 2 Dentatus has designed and researched use of SDIs using soft denture-relining material around the implants to support and retain mandibular complete dentures. The Atlas system uses four or more implants of appropriate length and of 2.2 mm or 2.4 mm in diameter, which the dentist places in the mandible at equal intervals anterior to the mental foramen. The dentist makes a complete mandibular denture and removes from it the interior portion in the location of the implants. He or she then lines this undercut space in the denture base with soft silicone denture-relining material, which surrounds the SDIs and retains and supports the denture. The dentist constructs the soft denture liner so that the patient can remove it for cleaning. This concept affords flexibility and movement of the denture in relation to the stress of masticating food. The soft liner can be replaced as it wears and becomes inadequate to retain the denture. The Sterngold Dental ERA Mini Implant System uses the well-known ERA attachment system, in which one part of the ERA attachment is incorporated into the denture base and the corresponding ERA component is placed on top of each of the four implants. The technique generally requires two smaller 2.2-mm–diameter implants in the anterior portion of the mandible and one 3.25-mm–diameter implant on each side of the arch in the area just anterior to the mental foramen. These four implants provide positive, stable retention and support for the denture and offer several levels of retention according to patient needs and the level of retentiveness of the ERA attachment placed into the denture. Conventional-diameter root-form implants (3 mm and larger in diameter) are one of the major advancements in dentistry’s history. However, they often cannot be used in patients who have minimal bone and who will not or cannot undergo bone grafting, patients who are unhealthy or patients who want minimally invasive procedures. The views expressed are those of the author and do not necessarily reflect the opinions or official policies of the American Dental Association. *Dr. Christensen is the director, Practical Clinical Courses, and a cofounder and senior consultant, CR Foundation, Provo, Utah. He also is the senior academic advisor, Scottsdale Center for Dentistry, Scottsdale, Ariz.; an adjunct professor, Brigham Young University, Provo, Utah; and an adjunct professor, University of Utah, Salt Lake City.
26: MDI ClinicalStudies from AroundTheWorld
Alessandria,Italy 2013 Mooresville,NC
MSplintedZirconiaFixedPartial DentureSupportedby Small Diameter (Mini Implants) in the Posterior Mandible: A Case Letter 2013. (Three 2.5 x12mm)
Andrea Mascolo, DDS1*
Paresh Patel, DDS2
Private practice, Alessandria, Italy.
2 Private practice, Mooresville, NC.
* Corresponding author, e-mail: andrea@studiomascolo.eu DOI: 10.1pxW
Journal of Oral Implantology 287 288 Vol. XXXIX/Special Issue/2013
http://www.joionline.org/doi/pdf/10.
1563/AAID-JOI-D-12-00043?code=aaid-premdev
The purpose of this case letter is to demonstrate that SPLINTED MINI IMPLANTS may successfully support a FIXED zirconia partial denture in the POSTERIOR mandible in highly selected patients and with an appropriate prosthetic design.
The use of 2 small- diameter (mini) implants can REDUCE the CANTILEVER effect created when using the procedure recommended by Misch (4-mm implant for a 7-mm mesial distal width).2
Three 2.5 x 12mm one- piece mini dental implants (OCO Biomedical, Albuquerque, NM) were placed.
In situations where there may be an inadequate interdental space, reduced interocclusal space, convergent adjacent tooth roots, close proximity of adjacent tooth roots, narrow atrophic osseous contour, and adequate osseous quality, mini implants may be appropriate to support a FIXED prosthesis in highly selected patients.3,4
In this case example, to reduce the potential for implant overload, the decision was made to use 3 mini implants SPLINTED together.
This would allow for an INCREASE increase in implant surface area while MINIMIZING the volume of bone removal during the osteotomy.
The final fixed restoration would also be designed with a narrow occlusal table to keep off axis forces to a minimum and to help prevent metal fatigue and cyclic-loading stress.
There are ADVANTAGES to using 2 to 3 mini implants to support a MOLAR restoration instead of a single wide-diameter implant.
Quite OFTEN , the loss of mandibular molars results in a mesial-distal dimension that is INSUFFICIENT in LENGTH for the placement of 2 conventional, standard-size implants.
The use of mini implants in this case letter allows for MINIMAL CANTILEVERS in the final restoration.
There is greater flexibility to maximize placement in compromised bone sites engaging the facial and lingual plates, and there may be BETTER RETENTION of CRESTAL BONE LEVELS around mini implants.5
However, the use of mini implants does have significant limitations, with reduced surface area being the foremost. When an occlusal force is applied, the strain to the supporting bone around small-diameter implants will be greater than a standard body implant.6–8
CONCLUSIONS
Splinted mini implants may successfully support zirconia fixed partial dentures in the posterior mandible in highly selected patients with an appropriate prosthetic design.
The implant dentist should consider MANY DIVERSE IMPLANT and PROSTHETIC DESIGNS to treat appropriately the ANATOMIC CONDITIONS with which patients present.
27: MDI ClinicalStudies from AroundTheWorld
Alessandria,Italy 2016
Small Diameter Implants (SDIs) in Fixed Restorations: Clinical Cases Considerations During 4 Years Follow-Up 2016
Andrea Mascolo* D.D.S, Master in Oral Surgery and Odontostomatological Urgency, Expert in Minimally Invasive Procedures,
Research & Reviews: Journal of Dental Sciences
RRJDS | Volume 4 | Issue 1 | March, 2016
Small diameter implants (SDIs), which were introduced to stabilize temporary dentures, were soon found to have several other clinical applications due to their high versatility [8,9]. For example, they have been used with a success in cases of limited interdental spaces [10,11]. Signi cant ndings have been reported in the literature about the long-term survival of small diameter implants [12,13]. Guidelines are available in the literature about the surgical techniques and rehabilitation, and several evidences suggest xed restorations with excellent long-term survival data [14,15]. Mini-invasive techniques offer both intraoperative and postoperative advantages, and they facilitate the healing of the tissues [16].
Some of the notable ADVANTAGES are as follows:
1. Quicker healing postoperatively
2. Decreased potential of future bone loss around SDIs for the one-body design
3. Simpler placement protocols
4. Decreased waiting period until nal prosthesis delivery compared to conventional implant treatment.
5. Anatomical limitations are lowered due to smaller diameters of the implants.
6. A less invasive implant treatment option for medically compromised patients.
The SDIs were loaded as follows: 5 SDIs were immediate loaded while 43 SDIs were loaded after 3 months considering the initial critical stability period around to 3 weeks and the osseointegration period of 3 months as suggested in the initial guidelines [14]. When the implants were loaded, the crowns and bridges were loaded with light contacts as with the conventional implants.
In attempts to reduce patient morbidity and convalescence, minimally invasive surgical techniques are becoming more and more discussed and practiced. Accurate planning and case evaluation are imperative for a success.
The VERSATILITY of the SDI offers the opportunity to propose an implant treatment to patients of wider ranges.
Failures in some cases have dissuaded some clinicians from using SDI’s. Some of these failures may have resulted from loading them too soon in areas with soft bone, use of implants of inadequate lengths, and or patients’ para-functional habits.
With DECREASED SURFACE AREA of the SDI’s, it is recommended to choose LONGEST possible implants without causing harms to surrounding vital structures [8,12-14].
The ADVANTAGES in certain situations, registered in the clinical experience have been:
• Multiple SDIs can offer an adequate surface area needed for a successful xed prosthetic.
• Engagement of the cortical plates in thin ridges for excellent primary stabilization.
• No micro-gap as the SDI’s are one body design.
• A apless approach to maximize the available blood supplies and reduce healing time
• A less amount of bone is removed per placement thus leaving more native tissue to disperse forces
• A pre-contoured abutment that can be shaped in vivo if needed
Conclusion
The clinical experience shows good performance of small diameter implants in xed solutions; the results are appreciated from clinicians and from patients for the minimal invasive approach and functional standpoint. During the follow-up period we have not registered peri-implant bone resorption; we have noticed healthy gingival remodeling around the implants. The reduced diameter of the abutments helps to secure a favorable remodeling of the soft tissues; the abutment connection is able to seal the perimplant area eliminating micro-leakages. The results achieved in the clinical trial encourage the use of small diameter implants in some clinical situations as example thin bony ridges and or limited interdental spaces, NOT just in anterior areas as initially proposed from earlier literatures. Some of the important factors for a success are: a clinically considerate patient selection, a planning according to the guidelines, and emphasizing judicious checking on occlusion after restoration is completed.
Figure 11. Initial clinical view.
Figure 12. Intra surgery: apless procedure no bleeding.
Figure 14. PFM restoration.
Figure 15. PFM restoration cemented.
Figure 16. Clinical revaluation 50 months.
28: MDI ClinicalStudies from AroundTheWorld
Tel-Aviv,Israel 2012
Replacement of a Molar With 2 Narrow Diameter Dental Implants 2012 Ziv Mazor, DMD,* Adi Lorean, DMD,† Eitan Mijiritsky, DMD,‡ and Liran Levin, DMD§
IMPLANT DENTISTRY / VOLUME 21, NUMBER 1 2012
http://planmed.com.tr/tr/kurumsal/
upload/yayinlar/yayin_03022013205017.pdf
The use of 2 implants to replace a single MOLAR seems a LOGICAL treatment solution to AVOID prosthetic complications.6,12
The aim of the present study was to present results of single molar area rehabilitated by 2 narrow diameter dental implants.
SINGLE regular-diameter implants might be incapable of predictably withstanding molar masticatory function and occlusal loading forces.
WIDE -diameter implants are a suitable alternative for replacing a missing MOLAR in some cases; however, the use of 2 implants has been successfully demonstrated to be a FUNCTIONAL and MORE BIOMECHANICALLY SOUND METHOD of MOLAR replacement.15
Wide-diameter implants are not always a treatment option for replacing a single molar, especially when the buccolingual dimension is deficient.
The USE of 2 IMPLANTS might also provide BETTER PROSTHETIC STABILITY and PREVENT ROTATIONAL FORCES on the prosthetic components.
Restoration of missing molars with 1 wide-diameter implant has a greater incidence of screw loosening16 and, compared with 2 implants, has a greater incidence of prosthesis mobility6 and a higher failure rate.17
When narrow implants are used as single- tooth replacement, especially in the molar region, an increased risk of screw loosening or fracture exists due to the combination of high masticatory forces, buccal-lingual mandibular movement, and cusp-groove orientation.18
Therefore, the use of 2 implants to replace a single molar is a logical treatment solution to avoid prosthodontic complications.12
One significant barrier to the widespread use of this concept is the limitation of the size of implants and their associated prosthetic components.
Nevertheless, when using narrow implants, 2 implants could be used even when the distance between the adjacent teeth is rather limited.
This case series provided an evidence for the usefulness of 2 narrow diameter implants to replace a single molar.
There is, however, a need for further long-term comparison studies to confirm and reaffirm the result pre- sented here.
Fig. 1. Replacement of a molar with 2 narrow dental implants. a, A missing first left molar with a mesiodistal distance of 11 mm (upper view) was replaced with 2 narrow diameter dental implants (lower view). b, The final rehabilitation consisted of a crown with an artificial intrara- dicular space (upper view—laboratory work). Note the final restoration in place where broad floss is inserted for cleaning the area in an intraradicular manner (lower view left). Final radio- graphic view is presented in the lower right view.
CONCLUSION
Replacing a single missing MOLAR with 2 narrow dental implants might serve as a viable treatment option providing good and predictable LONG-TERM RESULTS.
29: MDI ClinicalStudies from AroundTheWorld
Tel-Aviv,Israel 2004
Mini-Implants to Reconstruct Missing Teeth in Severe Ridge Deficiency and Small Interdental Space: A 5-Year Case Series 2004
Ziv Mazor, DMD,* Marius Steigmann, DMD,† Roy Leshem, DDS,‡ and Micahel Peleg, DMD§
https://www.academia.edu/22902650
/Mazor_Z_Steigmann_M_Leshem_R_et_
al._Mini-implants_to_reconstruct_missing
_teeth_in_severe_ridge_deficiency_and_
small_interdental_space_A_5-year_case_series
The purpose of this article is to describe the use of mini-implants for fixed restorations (with a follow up of up to 5 years) to enable the practitioner to overcome the anatomic obstacles of ridge width and narrow interdental space by immediate loading and reconstruction.
Two of the major obstacles for dental implant placement to replace missing teeth are the lack of adequate bone width and interdental space. Overcoming these limitations requires bone augmentation procedures that transform the deficient ridge into a ridge that is capable of receiving conventional tooth-form implants. In the case of inadequate interdental space, orthodontic tooth movement is advocated before implantation. Using narrow-diameter mini-implants allows the clinician to overcome both of these obstacles without the need for additional grafting procedures or orthodontic tooth movement.
The mini-implants are immediately loaded and restored so as to enable the patient to have satisfactory mastication and aesthetic appearance. A 5-year followup of 32 implants demonstrates the benefit of this treatment modality. (Implant Dent 2004;13:336–341)
The problem of ridge deficiency and interdental space can be solved with the use of narrow-diameter implants. Placement of mini-implants (1.8–2.4 mm in diameter) that are retrieved is a well-established procedure used to support fixed or removable prosthesis.
Mini-implants provide immediate FIXED provisional prosthe- sis, avoid premature implant loading, and protect augmented sites. In most patients, the transitional implants were retrieved at the time of implant uncov- ering, unlike the present clinical study in which implants were loaded imme- diately, maintaining function up to 5 years. This clinical study used mini- implants to reconstruct single missing teeth in narrow anterior and posterior ridges and narrow interdental spaces, are loaded immediately, then followed for 5 years.
CONCLUSION
Within the limits of this pilot study, the proposed treatment modal- ity of mini-implants may serve as a useful option to rehabilitate a single tooth in both deficient ridges and in narrow interdental spaces. Future studies should be conducted to evaluate the long-term survival of these implants.
30: MDI ClinicalStudies from AroundTheUSA
Utica,NY 2011
Small Diameter Implants: Specific Indications and Considerations for the Posterior Mandible: A Case Report
Journal of Oral Implantology 2011
DOI: 10.1563/AAID-JOI-D-09-00142.1
Brian J. Jackson, DDS* Private practice, Utica, NY. e-mail: BJJDDSIMPLANT@AOL. com
http://www.joionline.org/doi/pdf/
10.1563/AAID-JOI-D-09-00142.1?
code=aaid-premdev
The utilization of SMALL diameter implants in LIMITED osseous regions INCREASES patients’ ability to choose implants as a VIABLE RESTORATIVE OPTION.
Although SMALL diameter implants have been indicated in the incisor region for the maxilla and mandible primarily, their usage SHOULD BE CONSIDERED in select POSTERIOR regions.
These 2 case reports demonstrate the incorporation of small diameter implants to replace MISSING MANDIBULAR POSTERIOR TEETH.
Small diameter (1.8–3.0 mm diameter) implants have been widely accepted beause they can be utilized in regions of the mouth that are deficient in arch length, as well as alveolar width.1–3 Although small diameter single-stage implants have been indicated mainly for the maxillary lateral incisors and the mandibular incisor region, another clinical situation may warrant their application.
Loss of maxillary and mandibular molars results in a mesial-distal dimension that may be insufficient in length for the placement of 2 conventional, standard size implants (3.75 mm diameter). In addition, a single large implant (4.7 mm or 6.0 mm diameter) may demonstrate limitations caused by existing osseous structures or with regard to established implant occlusal principles.
The utilization of small diameter implants has become more widespread because of the demand for endosseous implants in a WIDE RANGE of OSSEOUS DIMENSIONS .
Although bone-grafting procedures can idealize the width of the alveolar ridge, many patients decline because of the additional time, cost, and morbidity. Additionally, bone-grafting procedures do not resolve the issue of length in the mesial-distal dimension. As a result, small diameter implants are being used as an alternative diameter choice to gain case acceptance.13 The main advantages of this type of endosseous implant are its size, 1-piece design, and precontoured abutment, as well as the ease of the restorative phase.14 Predictability in strength of the implant is largely due to the lack of an abutment-fixture connection (micro-gap) and retention screw commonly found in the 2-stage design.
Alternative surgical approaches to ideal- ize ridge width for incorporating standard size implants (3.75 mm) include block onlay grafting, ridge expansion, and/or alveolo- plasty. The surgical process of block onlay grafting leads to additional surgeries, as well as increased treatment time and costs and morbidity. Additionally, a secondary donor site is required, which involves risks of infection and parasthesia.17 The surgical concept of ridge expansion is possible in the maxilla but is limited in the mandible.18 Alveoplasty can widen the crest of the ridge but often is not an option in the mandible because of the proximity of the superior aspect of the inferior alveolar nerve and the density of the bone.
The 2-implant concept to replace a single MOLAR allows for an enhanced prognosis by INCREASING IMPLANT SURFACE AREA by SPLINTING .
Also, it eliminates the complication of abutment screw loosening by reducing detrimental rotational movements such as wobble or tipping.
In addition, it reduces the size of the gingival embrasures often present when a single implant replaces a mandibular first molar.
This clinical problem often becomes the patient’s chief complaint after final restoration placement.
Use of 1 implant per root has been recommended as the appropriate treatment plan for implant mandibular molar replace- ment.19
CONCLUSION
The field of oral implantology has become a widely accepted area of interest in dentistry.
The role of the dentist is to recommend treatment that is supported by research and leads to reduced treatment times, risks, and costs to patients.
Small diameter implants have become a viable alternative to standard conventional implants in a large number of clinical situations.
The mandibular posterior regions of the mouth may present an opportunity to incorporate these types of implants to reduce surgeries, morbidity, and treatment time.
Additionally, small diameter implants can increase the long-term prognosis of the prosthesis by increasing surface area and reducing screw loosening.
The precontoured abutment and impression copings make the restorative stage simple and effective for the experienced or novice practitioner.
It is critical that the clinician design the prosthesis in accordance with implant occlusal principles to maximize long- term success.
Although small diameter implants have been utilized in many mandibular clinical areas, additional long-term studies focused on maxillary and/or mandibular posterior regions of the mouth will lead to greater acceptance by clinicians.
31: MDI ClinicalStudies from AroundTheWorld
Kaunas, Lithuania 2012
New approach towards mini dental implants and small-diameter implants: an option for long-term prostheses.2012
Gleiznys A1, Skirbutis G, Harb A, Barzdziukaite I, Grinyte I.
Stomatologija. 2012;14(2):39-45
http://www.sbdmj.com/122/122-01.pdf
Conclusions.
Implants with SMALL DIAMETERS can be used SUCCESSFULLY in a variety of clinical situations. Less surgical time, less postoperative pain, ability of direct loading after surgery with no harm to bone and cost effectiveness are the advantages. The reduced surface implants require correct treatment planning so that the loading force would not cause bone loss or implant failure.
MDI and SDI show HIGH SURVIVAL RATES ,but special cautions for bone quality and good oral hygiene should be maintained.
However, nowadays, science, technology and number of researches have made it possible to improve our choice for better care of teeth and understanding the oral health leading to perfect deal with most of the oral problems. Osseointegration has become the main concept in modern implantology, this lead to introduction and refinement of the osseointegrated root form implant. Nowadays, available implants vary in diameter between 1.8 mm and 7 mm: implants with diameter less than or equal to 2.7 mm are called mini diameter implants (MDI) (1-5), while those of 3 to 3.3 mm (6, 7) diameter are called small diameter implants (SDI), and conventional implants are those up to 7 mm (1, 8). In the beginning,
After this had been found, the SDI and MDI have been approved for long-term use in 1997 by the FDA (8) resulting in avoiding bone augmentation or enlarging the mesiodistal space and giving the opportunity for more patients with severe cases to gain implant therapy. Conventional implants appeared problematic in: small space between the teeth in the place implant was supposed to be placed, in areas in which bone resorption had occurred, in cases where edentulous arches were with minimal bone in Table 2. MDI and SDI survival rates (continued on p. 42) a facial-lingual or mesiodistal direction, that could lead to excluding such patients from treatment (8). In order to place dental implant in partially edentulous patients, it has been recommended to maintain 2 mm to 3 mm of available space between the surface of the implant and the residual dentition to avoid impinging or damaging the periodontal ligaments of the adjacent teeth (9).
PRIMARY STABILITY of small diameter and mini-dental implants showed sufficiency for immediate loading, they can be used as an alternative to treatment with FIXED PARTIAL DENTURES in terms of both clinical and aesthetic criteria, as well for retention of complete maxillary and mandibular overdentures (20). Smaller diameter implants are preferred rather than conventional ones for REASONS of BLOOD SUPPLY, that is, conventional ional implants may disturb the blood supply to the bone around the implant (22). Additionally, IF there is adequate space and an unforeseen bone density or site inadequacy is encountered during the osteotomy of a small-diameter implant, the use of a slightly larger-diameter implant that is able to attain better initial stability stays an option (23)
CONCLUSIONS
Implants with SMALL DIAMETERS are one of the MAJOR ADVANCEMENTS in dental history; they can be used successfully in a variety of clinical situations. Researches continue to demonstrate the surgical and prosthodontic success of those implants. They offer patients satisfaction due to less surgical time, less postoperative pain and ability of direct loading after surgery with no harm to bone. Also they are more cost effective option, since they can support a denture with a reduced cost. It must be emphasized that the reduced surface implants require correct treatment planning so that the loading force would not cause bone loss or implant failure. Nevertheless, MDI and SDI showed HIGH SURVIVAL RATES , but special cautions of bone quality and good oral hygiene should be maintained. Due to simplified procedures, this could be a good choice for unexperienced dentists for their first steps.
32: MDI ClinicalStudies from AroundTheWorld
Markham, Ontario, Canada 2007
Applications of the Small-Diameter Implant in Dentistry
Ian Erwood,DDS
Inside Dentistry. Sept 2007. Special Issue 2
The use of small diameter implants SDI’s which are less than 3 mm in diameter is only recently gaining popularity for both FIXED and removable stabilization of a dental prosthesis as well as temporary anchorage for various applications in the dental field.
Small diameter implants SDI’s that are less than 3 mm in diameter have been in use in Europe for over 40 years and getting food and drug administration FDA approval for long-term use in 2003.
SDIs have only recently gained popularity among the North American dental community as a viable option for fixed removable temporary anchorage applications.
The long-term survival of MDI implants for a FIXED and removable prosthetics is SIMILAR to regular diameter endosseous implants.
Because MDI implants require less bone witdth,have an atraumatic surgery and placement ,can be loaded immediately ,and are more economical when compared to regular diameter and endosseous implants ,their use in oral rehabilitation will continue to rise.
33: MDI ClinicalStudies from AroundTheUSA
Utica,NY 2014
Fixed Partial Denture Treatment With Mini Dental Implants 2014
Brian J. Jackson, DDS
Journal of Oral Implantology Vol. XL/No. Six/2014
http://www.joionline.org/
doi/pdf/10.1563/
aaid-joi-
D-14-00037?code=aaid-premde
Very small diameter implants or mini dental implants (MDI) are a treatment alternative due to their reduced size. MDI does not require bone augmentation procedures, which are tech- nique sensitive, time consuming, and vary in predictable results.1,2 The option of utilizing MDI provides a minimally invasive, safe, and cost- effective approach for restoring the patient with deficient bone volume.3,4
The idea that very small diameter implants could osseointegrate and be used long term was conceived when retrieval was difficult or impossible without separation of the implant. Subsequent research supported that the biological phenomenon of osseointegration oc- curred on the surface of very small diameter implants.9,10 Recent research has demonstrated that mini dental implants can be utilized successfully to retain fixed multi-unit partial dentures.11,1
The concept of minimally invasive surgical proce- dures has escalated in the past several years. The option of mini dental implant therapy as an implant reconstruction modality aligns with this emerging idea.19 The flapless, non-bone grafting approach to implant surgery provides the patient with a safe, effective means for prosthetic reconstruction. The success
The biological concept of osseointegration has been established for very small diameter implants. Long-term survival depends on initial rigid fixation via thread design as well as the strength of the implant.20 The macrostructure thread design and roughene
Patients present with missing teeth with resultant bone loss. Dentists see this clinical situation worsen over time, with clinical management becoming more challenging, requiring extensive procedures prior to implant surgery. The utilization of very small diameter implants for highly selected patients can provide a minimally invasive, safe, and predictable alternative to conventional bone grafting proce- dures. Although the usage of very small diameter or mini dental implants (MDI) continues to evolve and expand, there exists a need for an increase in the body of research.
FIGURE 1. Initial intraoral-centric relation. FIGURE 2. Initial periapical radiographs. FIGURE 3. Initial intraoral- presurgical facial view. FIGURE 4. Surgical template. FIGURE 5. Bleeding points indicating future implant sites. FIGURE 6. Transgingival penetration with a #2 round surgical bur. FIGURE 7. Mucoperiosteal flap. FIGURE 8. (4) 2.1mm x 10mm collared square-head mini dental implants (MDI)-facial view.
FIGURE 9. (4) 2.1mm x 10mm collared square-head MDI-centric rich plasma (PRP). FIGURE 12. Mandibular left canine (#22) pre-extraction surgery. FIGURE 13. Mini dental implant (MDI) impression transfers. FIGURE 14. MDI impression transfers captured in polyvinyl siloxane material. FIGURE 15. Implant analogs/ transfers secured in impression material. FIGURE 16. 5-unit metal framework try in. FIGURE 17. 5-unit porcelain fused to metal- facial occlusal view. FIGURE 18. 5-unit porcelain fused to metal prosthesis-centric relation.
34: MDIClinicalStudies from AroundTheUSA
Pittsburgh,Pa 2006
USE OF MINI IMPLANTS FOR REPLACEMENT AND IMMEDIATE LOADING OF 2 SINGLE-TOOTH RESTORATIONS: A CLINICAL CASE REPORT 2006
Azfar A. Siddiqui, DMD, MSc Mark Sosovicka, DMD Mark Goetz, CDT
Journal of Oral Implantology 2 Vol. XXXII/No. Two/2006
http://www.joionline.org/doi/pdf/
10.1563/794.1
This article reports on the clinical use of mini implants in a patient with congenitally missing mandibular canines with limited mesiodistal bone dimension.
Dental implants are now considered the treatment of choice for replacement of all forms of tooth loss. Apart from providing function and esthetics similar to natural dentition, they also provide the most conservative treatment option, especially for single-tooth restoration. Until recently, dental- implant treatment was limited to patients with a minimum of 7 mm to 8 mm of available mesiodistal bone width to enable the placement of a 3.0-mm-diameter im- plant without impinging on the roots of the adjacent teeth. The availability of mini implants 1.8 mm and 2.2 mm in diameter, and FDA approval for use as definitive prosthesis support and retention, has opened new di- mensions in oral-implant restoration. Mini implants obviously have less surface area available for osseointegration compared to narrow-diameter implants, and this may be a handicap in some clinical situations. In the present case report, the patient’s minimal mesiodistal space precluded the use of narrow-diameter implants, but also presented a very favorable occlusal scheme that enabled immediate loading of two 2.4-mm-diameter implants with single-tooth restorations. Apart from a conservative approach and no adjacent tooth modification, additional benefits to the patient were reduced cost and fixed restorations.
CONCLUSIONS
Mini implants are indicated for areas where the use of narrow- diameter implants ( 3.0 mm) are contraindicated. Until long-term longitudinal clinical data on mini dental implants are unavailable, their use should be limited to areas with potentially less occlusal load.
FIGURE 1. Patient with congenitally missing mandibular canine teeth. FIGURE 2. Preoperative panoramic radiograph. Note the distal inclination of the lateral incisors. FIGURE 3. Right lateral contacts. FIGURE 4. Left lateral contacts. FIGURE 5. A crestal incision exposed the osteotomy site. FIGURE 6. The 1.0-mm drill with a rubber stopper at a predetermined length. FIGURE 7. A 2.4-mm- diameter mini implant initiated to engage the osteotomy. FIGURE 8. The implant was tightened using the titanium finger driver. FIGURE 9. A winged driver was used when increased resistance was felt. FIGURE 10. A ratchet was only used as a final step to submerge the implant threads. FIGURE 11. Both implants in position. FIGURE 12. Postoperative panoramic radiographs demonstrated the desirable positioning of both implants. FIGURE 13. A final impression was made at the time of surgery. FIGURE 14. Provisional crowns were placed on the day of surgery. FIGURE 15. Placement of the final, implant-supported crowns at the 2-week follow-up appointment.
35: MDI ClinicalStudies from AroundTheWorld 2006
Milan, Italy
Clinical and radiographic evaluation of small-diameter (3.3-mm) implants followed for 1–7 years: a longitu dinal study 2006
Eugenio Romeo Diego Lops Leonardo Amorfini Matteo Chiapasco Marco Ghisolfi Giorgio Vogel
Clin. Oral Impl. Res. 17, 2006 / 139–148
Cumulative survival and success rates of small-diameter implants and standard-diameter implants were not statistically different (P40.05).
Type 4 bone was a determining failure factor, while marginal bone loss was not influenced by the different implant diameters. The results suggest that small-diameter implants can be successfully used in the treatment of partially edentulous patients.
From the outcomes of the present study, using small-diameter implants seems to be a treatment option as predictable as using standard-diameter implants.
The cumula- tive survival and success rates of the two groups of implants were comparable, both for the maxillary and mandibular implants.
Narrow implants medium-term prognosis is comparable to the one of standard-diameter implants followed up in the present study.
Therefore, the high reliability of small-diameter implants is confirmed.
Standard and narrow implant prog- noses were influenced by peri-implant bone infection more than biomechanical factors, such as implant over- loading. Peri-implant bone resorption was not significantly influenced by different implant diameters (3.3 and 4.1 mm). Bone quality seems to be an impor- tant prognosis factor both for stan- dard- and small-diameter implants; spongy bone (type4)may increase implant failures. This trend needs to be confirmed by the clinical evaluation of a larger number of implants. (v) Survival of standard and narrow implants does not seem to be affected by implant location. However, because of the low number of implant failures observed in the current study, further research is required to elucidate the most appropriate implant distribution.
36: MDI ClinicalStudies from AroundTheWorld
Bologna ,Italy 2008
Clinical outcome of narrow diameter implants: a retrospective study of 510 implants. 2008
Degidi M, et al.
Authors
Degidi M1, Piattelli A, Carinci F.
Dental School, University of Bologna, Bologna, Italy.
J Periodontol. 2008 Jan;79(1):49-54. doi: 10.1902/jop.2008.070248 .
https://www.ncbi.nlm.nih.gov/pubmed/18166092/
Abstract
BACKGROUND: Narrow diameter implants ([NDIs]; diameter <3.75 mm) are a potential solution for specific clinical situations such as reduced interradicular bone, thin alveolar crest, and replacement of teeth with small cervical diameter. NDIs have been available in clinical practice since the 1990s, but only a few studies have analyzed their clinical outcome.
METHODS:
From November 1996 to February 2004, 237 patients were selected, and 510 NDIs were inserted. Implant diameter ranged from 3.0 to 3.5 mm, multiple implant systems were used, and 255 implants were restored immediately without loading (IRWL). No statistical differences were detected among the studied variables. Consequently, marginal bone loss (MBL) was considered an indicator of the success rate (SCR) to evaluate the effect of several host-, surgery-, and implant-related factors. A general linear model (GLM) was used to detect those variables statistically associated with MBL.
RESULTS: Only three of 510 implants were lost (survival rate [SRR] = 99.4%), and no differences were detected among the studied variables. On the contrary, the GLM showed that delayed loading and longer (>13 mm) and larger (3.4 and 3.5 mm) NDIs reduced MBL.
CONCLUSIONS:
NDIs have a HIGH SRR and SCR, SIMILAR TO those reported in previous studies of REGULAR DIAMETER IMPLANTS. Moreover, IRWL of NDIs is a RELIABLE PROCEDURE , although a slightly higher bone resorption is reported compared to delayed loading. No implant fractures were detected in the present series.
PMID 18166092 [
37: MDI ClinicalStudies from AroundTheWorld
Giza,Egypt
Peri-implant biomechanical responses to standard, short-wide, and double mini implants replacing missing molar supporting hybrid ceramic or full-metal crowns under axial and off-axial loading: an in vitro study 2017
Lamiaa Said Elfadaly*, Lamiaa Sayed Khairallah and Mona Atteya Al Agroudy
Correspondence: dr.l.fadaly@gmail.com
Fixed Prosthodontics, Cairo University, Giza, Egypt
International Journal of Implant Dentistry
Abstract
Background: The aim of this study was to evaluate the biomechanical response of the peri-implant bone to standard, short-wide, and double mini implants replacing missing molar supporting either hybrid ceramic crowns (Lava Ultimate restorative) or full-metal crowns under two different loading conditions (axial and off-axial loading) using strain gauge analysis.
Methods:
Three single-molar implant designs, (1) single, 3.8-mm (regular) diameter implant, (2) single, 5.8-mm (wide) diameter implant, and (3) two 2.5-mm diameter (double) implants connected through a single-molar crown, were embedded in epoxy resin by the aid of a surveyor to ensure their parallelism. Each implant supported full-metal crowns made of Ni-Cr alloy and hybrid ceramic with standardized dimensions. Epoxy resin casts were prepared to receive 4 strain gauges around each implant design, on the buccal, lingual, mesial, and distal surfaces. Results were analyzed statistically.
Results:
Results showed that implant design has statistically significant effect on peri-implant microstrains, where the standard implant showed the highest mean microstrain values followed by double mini implants, while the short-wide implant showed the lowest mean microstrain values. Concerning the superstructure material, implants supporting Lava Ultimate crowns had statistically significant higher mean microstrain values than those supporting full-metal crowns. Concerning the load direction, off-axial loading caused uneven distribution of load with statistically significant higher microstrain values on the site of off-axial loading (distal surface) than the axial loading.
Conclusions:
1.Implant design, superstructure material, and load direction significantly affect peri-implant microstrains
2. The recorded compressive and tensile microstrains for the tested designs were within the physiologic loading range, as they did not exceed the compressive or tensile strength of the bone-implant interface, which is more than 3000 microstrains ex- cept for the standard sized implant supporting Lava Ultimate crowns under both loading directions.
3. Off-axial loading leads to uneven distribution of loads, in standard diameter implant, due to the cantilever effect, which caused microstrain values exceeding the physiologic limit, thus causing clinical failure over time.
4. Use of splinted double mini implants and short-wide implant to restore missing mandibular molar duces cantilever effect which leads to lowering of peri-implant microstrains under off-axial loading.
5. Usage of full-metal crown implant superstructure re- duces the peri-implant microstrain values compared to using Lava Ultimate crowns.
38: ClinicalStudies from AroundTheUSA
New York, NY 2016
Use of Narrow-Diameter Implants in Treatment of Severely Atrophic Maxillary Anterior Region With Implant- Supported Fixed Restorations 2016
Stuart J. Froum, DDS; Sang-Choon Cho, DDS; Salvatore Florio, DDS; and Craig M. Misch, DDS, MDS
Compendium May 2016
Volume 37, Issue 5
Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
https://dentatususa.com/wp-content/
uploads/2016/11/126_May_2016_Froum1.pdf
Jun. 1 2016 12:54:24 PM]
Abstract:
The edentulous anterior atrophic maxilla represents a CHALLENGE for the surgeon and restorative dentist. Soft- and hard-tissue augmentation procedures are OFTEN REQUIRED prior to, or simultaneously with, implant placement. A well-planned treatment protocol, patient compliance, and collaboration between the treating clinicians and the laboratory are requirements in achieving predictable long-term outcomes that satisfy patient expectations. Avoiding transmucosal loading and movement of the graft during the healing phase are crucial factors in achieving lasting success.
In this case report, a fixed provisional restoration supported by four immediately loaded narrow-diameter implants (NDIs) was used to enable function during healing and protect the grafted site. Two of the NDIs, along with three conventional-diameter implants, were subsequently used to support the final restoration. NDIs with diameters of less than 3 mm can achieve excellent long-term osseointegration and may be used together with conventional implants for definitive prosthodontic treatment as demonstrated
Placing implants in prosthetically ideal positions in the atrophic maxilla is challenging and often requires soft- and hard-tissue augmentation procedures prior to, or simultaneously with, implant placement.1,2 Considering the complexity and treatment time, correct sequential planning is crucial to achieving predictable long-term results while satisfying the patient’s expectations for function and esthetics.
The use of narrow-diameter implants (NDIs) presents an invaluable modality for restoring an edentulous atrophic maxillary area in the provisionalization, augmentation, and final restorative phases of therapy.
All NDIs in this case report were category 1, according to the Klein classification, and are defined as implants with a less-than-3-mm diameter.3
These implants have been used to support removable and fixed dental prostheses since they were introduced in 1994.4
Among the articles that have been published on NDIs reporting SURVIVAL RATES COMPARABLE with conventional implants, Klein et al,3 in a systematic review of the literature, reported NDI survival rates between 90.9% and 100%.
The original function of NDIs was to support fixed interim prostheses during the osseointegration phase of conventional implants to avoid transmucosal loading that could compromise the final outcome. Following this initial healing period, the NDIs would be removed. It was later reported that the removal of these implants could be difficult because of the various degrees of integration they achieved.5 Froum et al6 confirmed this finding in a histologic study with machined-surface transitional implants. They analyzed the percentage of bone-to- implant contact (BIC) for NDIs after an average functioning period of 10.8 months. The values obtained were similar to the percentage of BIC of conventional turned, machined-surface implants. The results indicated that NDIs were able to achieve the same degrees of integration as implants with conventional diameters.6
Figure 6 & 7
Figure 8
Figure 9
Figure 10
Figure 11
Figure 12
Figure 13
Figure 14
In 2004 the US Food and Drug Administration approved the use of NDIs in the human jawbone for long-term use.7 Several authors have showed successful results when NDIs were used to support definitive prostheses.8-12 Furthermore, in a 2013 systematic review, Bidra and Almas13 reported a 94.7% survival rate of NDIs (diameter <3 mm) when used exclusively for definitive prosthodontics treatment. NDIs have been successfully used to support both transitional and fixed prostheses, thus providing clinicians with a simplified treatment option in areas of limited alveolar bone dimensions. In addition, they typically cost less than conventional implants and, in many cases, are able to be placed with a flapless procedure, which decreases patient postsurgical discomfort and morbidity.
Figure 15
Figure 16
Figure 17
This case report presents an 11-year follow-up of a patient in whom NDIs were used to support both the provisional and final restorations. The planning and sequencing of the procedures, including provisionalization, ridge augmentation, and final NDIs-conventional implants– supported restorations, will be discussed to illustrate the use of NDIs in the various phases of treatment. Case Report In 2004, a 30-year-old male was referred to the Ashman Department of Periodontology and Implant Dentistry of New York University College of Dentistry. The patient was a nonsmoker with an unremarkable medical history. His chief complaint was discomfort with his existing six-unit removable partial denture (Nos. 7 through 12), which he said he “could not tolerate” (Figure 1). He desired a fixed prosthesis. Two years earlier, severe trauma to the anterior maxilla had caused the loss of teeth Nos. 7 through 12 and the subsequent loss of supporting bone and soft tissues (Figure 2 and Figure 3). A computerized tomography scan revealed a deficient volume of buccolingual crestal bone and the need for a bone regeneration procedure prior to implant placement. The treatment plan was to first provide the patient with a fixed provisional restoration that would afford function and protect the planned grafted site. Four NDIs were planned to support an acrylic provisional prosthesis prior to the augmentation procedure and during the healing period. This was to be followed by replacement of two of the NDIs with three conventional-diameter implants to support the definitive prosthesis.
Figure 18
Surgical Procedures
Placement of four NDIs (1.8 mm x 14 mm) (ANEW®, Dentatus, www.dentatus.com) guided by a CAD/CAM surgical template (iGuide, Midwest Dental Arts, www.midwestdentalarts.com) was performed without flap elevation (Figure 4 and Figure 5). A single 1.4-mm pilot drill (CePo®, Dentatus) was used to prepare the osteotomy under copious irrigation at 1000 RPMs. The four NDIs were subsequently inserted at low speed (30 RPM) in position Nos. 7 through 9 and 12 (Figure 6 and Figure 7). Primary stability was tested with a torque driver and found to be sufficient for immediately loading the implants. Following placement of the NDIs, the patient’s provisional restoration was connected chairside. The design of the ANEW implants allowed fabrication of a screw-retained fixed restoration that was retrievable. Four openings were drilled in the patient’s acrylic prosthesis to ensure proper fit. A coping was attached to each of the four NDIs and secured in place with a screw cap. This coping assembly was then processed into the partial restoration using a self-curing acrylic resin (Bosworth TrueRepair®, Keystone Industries, www.keystoneindustries.com). The access holes for the screws were blocked with cotton pellets and sealed with off-color resin for easy re-access (Figure 8).
The bone augmentation procedure was performed 2 months following implant placement. The patient was given a prescription of amoxicillin 2000 mg 1 hour prior to surgery. Because of the large dimension of the horizontal defect, both allogeneic bone block grafts and autogenous
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5bone blocks, harvested from the right ascending mandibular ramus, were used. Crestal and intrasulcular incisions were made in the regions of teeth Nos. 6 through 15 around all teeth and NDIs. The autogenous bone block was sectioned in two pieces and shaped to eliminate sharp corners. After decortication, the two segments were fixated using two screws (OsteoMed, www.osteomed.com) in the region of missing teeth Nos. 7 through 10. The allogeneic bone block, which was also shaped, was fixated after decortication with two screws on the buccal aspect of missing teeth Nos. 10 through 12. The spaces were filled with particulate allogeneic graft (Puros Cancellous Particulate Allograft®, Zimmer Dental, www.zimmerdental.com) to obtain a homogenous surface (Figure 9). The grafted area was covered with two resorbable collagen membranes (Bio-Gide®, Geistlich Pharma, www.geistlich-pharma.com) that were stabilized with five tacks (truFIX, ACE Surgical, www.acesurgical.com) (Figure 10). A periosteal releasing incision was made to achieve tension-free closure using resorbable sutures (Coated Vicryl® 4.0, Ethicon, www.ethicon.com). To prevent transmucosal pressure on the tissues, which may have interfered with the healing process and the integration of the bone grafts, the buccal flange of the provisional was trimmed (Figure 11). Following surgery, amoxicillin 500 mg TID for 10 days and chlorhexidine 0.12% mouthrinse (PeridexTM, 3M ESPE, www.3MESPE.com) BID for 2 weeks were prescribed. The healing process was uneventful. Five months later, the block grafts appeared well integrated, and no signs of inflammation or bone resorption were noted. Two of the four NDIs (Nos. 7 and 12) were retained as planned and supported the provisional, while the other two (Nos. 8 and 9) were removed and replaced with three standard-diameter implants (3.5 mm x 13 mm) (Zimmer Dental) in sites Nos. 8, 9, and 11. Healing abutments were connected to these three implants (Figure 12). Due to a partial resorption of the allogeneic block graft, implant No. 11 was placed slightly more apical than Nos. 8 and 9, and a guided bone regeneration procedure was performed simultaneously using particulate allogeneic graft (Puros Cancellous Particulate Allograft) and a resorbable collagen membrane
Figure 6 & 7
Figure 8
Figure 9
Figure 10
Figure 11
Figure 12
Figure 13
Figure 14 (Bio-Gide). The flap was sutured with absorbable 4-0 chromic gut sutures (Ethicon). The augmented area was submerged while implants Nos. 8 and 9 and their healing abutments were left exposed (Figure 13). The provisional was relined with TrueRepair to close the access holes through which NDIs Nos. 8 and 9 had been connected to the restoration and to cover the two non-submerged healing abutments. At this stage, the provisional remained connected and supported only by two NDIs (Nos. 7 and 12). Four months later, a new provisional, supported by all five implants, was delivered (Figure 14). Once the healing of the soft tissues was completed, the final impression was taken and the final restoration was delivered (Figure 15).
Follow-up
Figure 15
Figure 16
Figure 17
Eleven years later, the patient, who lived in London, returned to the New York University periodontology and implant dentistry department for follow-up. Radiographic evaluation demonstrated complete implant integration with no bone resorption around either the standard-diameter implants or the NDIs (Figure 16). One of the titanium tacks that secured the membrane had remained above the No. 7 NDI. Because the tack was well tolerated with no hard- or soft-tissue pathology, it was allowed to remain in place. Clinically, no signs of soft-tissue inflammation were noted (Figure 17 and Figure 18), and the patient reported complete satisfaction with the function and esthetics of his fixed restoration. Discussion Implant treatment in an extremely atrophic maxilla is challenging for clinicians and requires careful evaluation, planning, and execution to achieve long-term success and fully satisfy the patient’s expectations. The surgeon, restorative dentist, and laboratory technician must work in collaboration to achieve the desired outcome. In the present case, the patient’s desire was to replace his removable partial denture with a fixed restoration. Oftentimes, patients do not tolerate removable prostheses well, especially when the tooth loss was sudden and caused by trauma or hopeless teeth need to be removed. Furthermore, when augmentation procedures are necessary, regardless of the final restorative options, protecting the grafted area and maintaining graft immobilization are essential to achieve success.14 Using a fixed provisional restoration is usually preferable, but many times this entails preparing healthy teeth to function as abutments. Another option is to immediately load the implants; however, this risks complications and failure when implants are placed in augmented sites.
Figure 18
A more predictable option is the use of NDIs, which can be placed in residual bone and support a fixed provisional restoration during the first phase of restoring function and during the time necessary for graft healing. The NDIs in the Nos. 7 and 12 positions were retained in the final prosthesis for the following reasons: First, they supported the provisional while the conventional-diameter implants— Nos. 8, 9, and 11—were allowed to integrate, which avoided transmucosal loading and provided a fixed provisional. Second, the width gained following block grafting in the No. 12 area was insufficient to place a conventional-diameter implant and still maintain at least 1 mm of buccal bone. Third, these implants continued to be stable with no bone loss and were, therefore, included as abutments in the final splint. Narrow-diameter implants are designed to be placed with a nonsubmerged protocol and then immediately loaded to support fixed interim prostheses.15 Findings from histologic studies have confirmed their bone integration at the light microscopic level, and their removal has been noted to be difficult.5,13 In a systematic review of the literature, Klein et al3 reported a survival rate between 90.9% and 100% for implants with diameters of less than 3 mm (the mean functional follow-up ranged between 12 and 96 months). Shatkin and Petrotto11 in a retrospective analysis of 5640 mini implants supporting fixed and removable prostheses found an overall implant survival rate of 92.1%. Although NDIs were originally introduced to support provisional restorations, the Food and Drug Administration, considering high-survival–rate data, approved their use for long-term prosthodontic treatment in 2004.7
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Although some in vitro studies16,17 reported a higher risk for overload and fracture for NDIs, these findings have not been confirmed clinically. When NDIs are used properly, long-term success without complications can be achieved, as this report demonstrates. Using an increased number of implants was suggested to overcome the risk for overload complications.16 A more predictable alternative is to splint NDIs to conventional- diameter implants. This strongly reduces stress levels in the surrounding bone tissue18,19 and may provide a more even distribution of strains during off-axis loading that could occur clinically.20 While the 11-year follow-up in the present case report demonstrates that long-term success could be achieved using this protocol, patient compliance played a key role in the outcome. In addition, the London dentist reported that the patient had professional dental maintenance every 3 months while in London. The patient’s oral hygiene was optimal for the duration of the treatment and then for years following the delivery of the final restoration. The patient also followed post-surgery instructions to not chew on the provisional or overload the implants for 3 to 4 months. The patient’s expectations were fully satisfied, and he was grateful for the treatment received. Conclusion Maxillary atrophic anterior ridges represent a challenge for the surgeon and restorative dentist. A well-planned treatment protocol, based on the close collaboration between the treating clinicians and laboratory, is a prerequisite for success. Through the careful evaluation and planning of the case, the clinicians must assess the advantages and disadvantages of the various therapy alternatives, selecting the most appropriate option to achieve long-term success and satisfy patient expectations. When bone-regeneration procedures are needed in order to place and restore an implant-supported restoration, various techniques have shown a high percentage of success. A requirement for effective bone regeneration is the avoidance of loading and movement during the healing process. A fixed interim restoration supported by NDIs protects the augmented site and represents a more comfortable and acceptable solution for most patients when compared to a removable denture. The use of NDIs presents a valuable modality in supporting fixed provisionals and does not require adjacent teeth to be prepared. Furthermore, these implants achieve excellent osseointegration and may be used long term to support the definitive prosthesis when splinted to standard- diameter implants.
About the Authors
Stuart J. Froum, DDS
Clinical Professor and Director of Clinical Research Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
Private Practice
New York, New York
Sang-Choon Cho, DDS
Clinical Assistant Professor
Director of Advanced Program for International Dentists in Implant Dentistry, and Co- Director of Clinical Research
Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
39: MDI ClinicalStudies from AroundTheWorld 2010
Germany,England
linical evaluation of Tiny® 2.5- and 3.0-mm narrow-diameter implants as definitive implants in different clinical situations: a retrospective cohort study. 2010
Anitua E, Errazquin JM, de Pedro J, Barrio P, Begoña L, Orive G.
Eur J Oral Implantol. 2010;3:315-322.
Authors
Anitua E1, Errazquin JM, de Pedro J, Barrio P, Begoña L, Orive G.
Author information
1
eduardoanitua@eduardoanitua.com
Citation
Eur J Oral Implantol. 2010 Winter;3(4):315-22.
Germany,England
Abstract
AIM: The aim of the present study was to assess retrospectively the survival of narrow-diameter implants (2.5 and 3 mm in diameter) in patients with insufficient bone ridge thickness for placement of standard-diameter implants.
MATERIAL AND METHODS:
Fifty-one patients with 89 inserted narrow-diameter implants (2.5 and 3.0 mm) were included. Patients were treated with one or more narrow-diameter implants between June 2004 and December 2005. The observation period for all included implants was at least 3 years after implant loading. Outcome measures were implant survival, complications and marginal bone level changes evaluated on panoramic radiographs.
RESULTS:
The mean follow-up period for all implants was 48 months. Only one implant was lost, yielding survival rates of 98.9% and 98.0% for the implant- and subject-based analyses, respectively. Six complications were reported. Twenty-four months after implant insertion, mean bone loss was 1.26 mm (SD 0.51).
CONCLUSIONS:
Narrow-diameter implants can be successfully used to treat narrow bone ridges up to 3 years after loading
40:MDI ClinicalStudies from AroundTheWorld:
Novi Ligure, Italy
Mooresville ,NC 2016
Minimally invasive implant therapy in geriatric patients using small diameter implants 2015
Drs. Paresh B. Patel and Andrea Mascolo explore the benefits of mini dental implants for senior patients
Implant practice
Volume 4 Number 4
July 2015
Dr. Paresh B. Patel
He practices in Mooresville, NC.
Dr. Andrea Mascolo
He maintains a private practice in Novi Ligure, Italy
Introduction
Several studies demonstrate high implant survival rates, a relatively low need for recurrent care, and improved quality of patients’ lives. This modality is an accepted treatment option for all ages.1,2 Consequently, implant-supported prosthodontic rehabilitation for function and esthetics is indicated more frequently. The aging population is growing, and these older adults have more teeth and more oral problems than previous generations. In 1900, 4% of the population was 65 years or older; by 2005, that number had increased to 12.4%, a 10-fold increase.3 It is expected by 2030 that some 70 million Americans will be over the age of 65, and many will have osteoporosis, diabetes, heart disease, and other health problems. All of these issues may pose challenges for implant dentists by making treatment decisions more difficult and complex. In2007,theAmericanAcademy of Implant Dentistry stated that as the population ages, dentists will see an increase in the number of elderly patients seeking dental implants. New solutions to combat these complex medical conditions in the geriatric population will be required.
Minimally invasive surgical procedures, applied to implantology, could play a key role in the treatment of this population.
This concept of reduced surgery can be facilitated by the use of CBCT, surgical guides, and flapless procedures. Mini dental implants are easy to place and can be used for a variety of prosthetics.4
Originally introduced 15 years ago to stabilize dentures, they now have been used in several other clinical applications, such as successfully restoring missing teeth with SINGLE or MULTIPLE-UNIT ,splinted,FIXED-partial dentures (FPDs).
The procedure for mini-implant placement is typically flapless, and requires less surgery than traditional implant protocols. With less surgery, the reported complications are extremely low.5
Other advantages include that SYSTEMIC contraindications are greatly reduced.
Patients with controlled diabetes, autoimmune disorders, osteoporosis, and cigarette use can now be considered for implant therapy. This could include geriatric patients, patients with anxiety, dental phobics, and patients with bleeding disorders.
Evidence shows that mini implants have excellent results with a 5-year and 7-year overall survival rate of more than 90%.6,7
It is expected that number will increase as correct placement protocols are established. A recent literature review highlights that PRIMARY STABILITY is a prerequisite for long-term success.8,9
If functional loads are correctly managed, secondary stability will occur, and osseointegration will be maintained.17 Bone quality is another important factor in determining the predictability of long-term success with mini dental implants. Type I and Type II bone are required for immediate loading and reduced healing times. Type III bone requires increased healing time and great care when applying functional load. Type IV bone is contraindicated for this procedure.6,7,10-12
The minimum number of mini implants required for appropriate retention of a complete removable denture may be SIX in the maxilla and FOUR in the mandible.6,9,13,14
The protocol for the restoration of ANTERIOR teeth should be ONE mini implant for each tooth.
In the POSTERIOR region, TWO mini implants shouldused to INCREASE the implant-to- bone SURFACE AREA when considering a fixed crown.
All prostheses, fixed or removable, require a CAREFUL ANALYSIS of the OCCLUSION to minimize and REDUCE AXIAL FORCES.6,7,12,15,16
The proposed protocols for mini- implant prostheses require a greater number of implants than conventional techniques, and a more accurate assessment of the position and angles to better distribute occlusal forces.
A rehabilitation of the UPPER ARCH, for example, would include SIX mini implants to support a FULL DENTURE while 10-12 mini implants are recommended for a FIXED SOLUTION .
SPLINTING the superstructure in the FIXED prosthesis results in a REDUCTION of Micro-Movement when load is applied.
According to the literature, MICRO-MOVEMENT is responsible for FAILURE in immediate loading.
Several studies demonstrate the long-term success of full-arch fixed prostheses supported by mini implants.6
Conclusion
The demand for MINIMALLY INVASIVE DENTISTRY is growing from both clinicians and patients. This concept, applied to implantology, offers advantages intra-operatively, postoperatively, and during the healing process.
It also offers considerable advantages to patients with SYSTEMIC CONDITIONS. “Progressive treatment planning” is a new concept and incorporates the use of mini implants. This will allow the treatment of geriatric patients through progressive steps. When patients present with edentulous areas combined with a restoratively and functionally sound dentition, mini Figure 8: Mini implant bridge 1 month post-op implants are well suited to support both removable and fixed solutions. As time, function, and age continue their relentless effects on the oral cavity, additional mini implants can easily be placed to support a larger prosthesis when needed. The progressive treatment plan is founded on the demands of patients but takes into consideration the physical response to mini implants and the capacity to maintain oral hygiene. Mini implant-retained dentures offer functional advantages in chewing and stability. In geriatric patients, where manual skills are often reduced, having a removable appliance can allow for proper hygiene maintenance. However as this geriatric population ages, insertion and removal of a multi-implant-supported prosthesis often is quite difficult, due in most cases to lack of physical force required. At this point, a fixed solution may provide better function and better compliance in oral hygiene.
This staggered approach of the progressive treatment plan allows patients to function properly, and gradually brings the patient, when possible and requested, to the IDEAL GOAL in prosthodontics :a FIXED SOLUTION.
41:MDI ClinicalStudies from AroundTheUSA
Pittsburgh,Penn 2012
A COMPARISON OF NARROW-PLATFORM (3.0-3.6mm) vs WIDER PLATFORM (3.7-6mm) DENTAL IMPLANTS
by Husain Alarfaj
BS, University of Pittsburgh, 2002 DMD, University of Pittsburgh, 2006
Submitted to the Graduate Faculty of
the School of Dental Medicine in partial fulfillment of the requirements for the degree of Master of Dental Science
University of Pittsburgh
2012
Flanagan 2008 (17) suggested the use of small diameter implants in compromised, narrow, or restricted sites in the posterior segments of the mandible and the maxilla. His studies analyzed and supported the use of small diameter implants (1.8-3.3mm) in the edentulous area. The study also recommended the splinting technique when the restorative phase comes into place. A small diameter implant poses less of an obstacle for angiogenesis and less percutaneous exposure and bone displacement as compared with standard-sized implants. In posterior sites, rounded and narrow prosthetic teeth present small occlusal tables to minimize axial and off-axial directed forces. Other factors influence the success rate of implant survival. Marginal bone loss is essential in determining the success or failure of an implant. Research at the University of California Department of Restorative Dentistry showed clearly that other factors are certainly involved affecting implant stability, survival rate and marginal bone loss (18). In research by Degidi 2008, 510 single small-diameter implants (3.0-3.5mm, 237 patients) were examined retrospectively from 1996-2004. Implant sites included all tooth position and had been functional eight years. Only three implants among the 510 failed, in this research the definition of failure being large amounts of marginal bone loss around the implant platform (19).
HYPOTHESIS
Narrow-platform implants (3.0-3.6mm) are as successful as wider-platform dental implants (3.7- 6mm) in the posterior region (molars and premolars).
The foundation of any structure or building has to be solid and architecturally sound to withstand any exerted force from any direction. The bioengineering of dental implants have always favored wide diameter dental implants. Logic says the wider the surface, the better tolerance of withstanding forces exerted on the crown, which extends to the dental implants. Major dental advancements have led dental implants to remarkably high routine success rates. Advancements in technology have introduced the ability to restore severely compromised sites such as knife edge boney structures or those with minimum boney volume bucco-lingually. Expectations for narrow diameter dental implants have flourished due to their improved success. Results of this study show that narrow diameter dental implants can indeed be used in the posterior area when boney volume is minimized. The results are close in value between the two major groups and statistically significant. The difference between mean values at BASELINE is 0.20 mm, 0.04 mm for the standard deviation. In other words, the healing process for narrow- platform and the regular/wide-diameter implant is very similar. However, after at least one year of function the gap between the values widened. The narrow-diameter dental implants have a mean value of 3.36mm with 0.58mm standard deviation whereas the regular/wide-diameter dental implants have a mean value of 3.05mm with 0.60mm standard deviation. The marginal bone level dropped to 0.60mm on average per year after at least one year of functional loading.
It was evident that the rate of bone loss for the two groups was consistent, with a slight elevation of bone loss observed in the narrow-diameter dental platform. In addition, both groups had upper and lower bounds for 95% confidence intervals ranging from 2.40mm to 3.20mm. Recent studies have shared similar results showing the ability of narrow-diameter dental implants to restore such areas. Romeo and Amorfini (4) have shown a draw between narrow- diameter and regular-diameter implant success. Research by Cordioli et al (2004) showed relatively good success for narrow-diameter implants in the restoration of single teeth in the premolar area (12). Flanagan 2008 (17) also suggested the use of small diameter implants in compromised, narrow, or restricted sites in the posterior segments of the mandible and the maxilla. His studies analyzed and supported the use of small diameter implants (1.8-3.3mm) in the edentulous area. A small-diameter implant is a less of an obstacle for angiogenesis and there is less percutaneous exposure and bone displacement as compared to standard-sized implants. Most new research and literature support and confirm the results in this study.
CONCLUSION
This research presents clear evidence of the success of the narrow-diameter dental implants restoring posterior edentulous area in the maxilla and the mandible. The data is statistically significant. The rate of bone loss around the narrow-diameter dental implants is slightly higher than the rate of bone loss around regular/wide-diameter dental implants. This may or may not have a direct clinical impact. In other words, those values are statistically significant but clinically not significant. To confirm these preliminary findings and indications, further prospective future research is necessary.
42: MDI ClinicalStudies from AroundTheWorld
Unionville,Ontario, Canada 2014
2014
An efficient treatment option when space is limited
Ian Erwood, BSc, DDS
Private Practice
Unionville, Ontario, Canada
InsideDentistry
January 2014
Volume 10, Issue 1
https://www.aegisdentalnetwork.com
/id/2014/01/mini-dental-implants-for-
single-crown-restorations
Ian Erwood, BSc, DDS
Regular diameter endosseous dental implants (>3.0 mm in diameter) restored with a crown have become the treatment of choice for single missing teeth in most cases.1-3 However, when replacing mandibular incisors and maxillary lateral incisors, or restoring locations where surrounding teeth may have migrated into edentulous areas, there is often inadequate space to place traditional implants without compromising the surrounding bone. A solution in cases when there is less than 7 mm of interdental space is the placement of a small-diameter implant (<3.0 mm), also known as a mini dental implant (MDI). These one-piece implants have been successfully used for the long-term stabilization of both complete and partial dentures. They range in diameter from 1.8 to 2.9 mm and in length from 10 to 18 mm, and can have either an O-ball or tapered prosthetic abutment. Due to the excellent primary stability achieved by MDIs and the proliferation of CAD/CAM tools, it is now possible to complete the entire procedure in a single office appointment. Case Presentation The patient had his upper left first premolar extracted approximately 5 years ago. There was buccal bone resorption (Figure 1) and a distance of 7 mm between the canine and the second premolar (Figure 2). After evaluation and consultation, the patient elected to have an MDI inserted and restored immediately with a full-crown restoration. At the placement appointment, the patient rinsed with chlorhexidine gluconate, and local infiltration anesthesia was administered. A 1.1-mm pilot drill at 1200 rpm was used to create a pilot hole. A 2.4-x-15-mm collared O-ball 3M™ ESPE™ MDI Mini Dental Implant (www.3mespe.com) was inserted and hand-screwed to achieve initial stability. A winged thumb wrench was then used to continue to insert the implant (Figure 3), and an adjustable torque wrench was used to verify that it was placed with at least 35 Ncm of force and was ready to be loaded. An impression and shades were taken and sent to a nearby dental laboratory. An MDI lab analog was placed in the impression and poured in die stone. The laboratory technician created a reduction coping for the head of the O-ball to ensure a path of insertion for the crown. The resulting die was scanned with a CEREC® CAD/CAM system (Sirona, www.sirona.com) and a crown was milled using 3M™ ESPE™ Lava™ Ultimate Restorative block and customized with indirect lab staining. The reduction coping was then used to trim one side of the O-ball. The crown was seated on the O-ball and the fit, shade, and occlusion were confirmed. The patient approved of the crown and the area was prepared for the final crown cementation. The area was isolated with a dry angle and cotton rolls, and a small piece of rubber dam (Figure 4) was placed over the O-ball and tucked around the implant collar. 3M™ ESPE™ Scotchbond™ Universal Adhesive was applied to the O-ball to enhance the bond strength of the cement. A thin layer of 3M™ ESPE™ RelyX™ Ultimate Adhesive Resin Cement was applied to the inside of the crown, which was then seated on the O-ball head. The crown was light cured for 3 seconds and excess cement was removed. After the cement had completely set, the area was re-evaluated to confirm the crown was slightly out of occlusion, which is preferred because there is no periodontal ligament compression as there is with the surrounding teeth. A final radiograph was taken (Figure 5), and the patient was given postoperative care instructions. The patient returned 1 week after the implant and crown were inserted to report that he had no discomfort and was pleased with his new tooth (Figure 6).
Conclusion
As this case illustrates, in areas where there is inadequate space for a regular diameter endosseous implant, a mini dental implant can be considered. Furthermore, in cases where the occlusal forces can be minimized, an immediate final or temporary crown can be placed, significantly shortening the traditional treatment process. Disclosure Dr. Erwood presents lectures on 3M ESPE Mini Dental Implants.
43:MDI ClinicalStudies from AroundTheWorld
Shanghai, China
Long-term outcomes of narrow diameter implants in posterior jaws: A retrospective study with at least 8-year follow-up 2018
Jun-Yu Shi† | Feng-Yuan Xu† | Long-Fei Zhuang | Ying-Xin Gu | Shi-Chong Qiao | Hong-Chang Lai
Department of Dental Implantation, Shanghai Key Laboratory Stomatology, Shanghai
Ninth People’s Hospital, Shanghai Jiaotong University, School of Medicine, Shanghai, China
Abstract
Objective: The aim of this study was to evaluate the long-term survival, complications, peri-implant conditions, marginal bone loss, and patient satisfaction of fixed dental prostheses supported by narrow diameter implants (NDIs) in the posterior jaws. Materials and methods: This study was designed as a retrospective cohort study with a mean follow-up time of 10.1 years (SD: 2.5 years). Patients receiving NDIs in poste- rior jaw were reviewed. Implant survival, hardware complication, modified plaque index (mPI), peri-implant probing depth (PPD), percentage of bleeding on probing (BOP%), marginal bone loss (MBL), and patient satisfaction were evaluated. Log-rank test and t test were used to detect the influence of implant location and restoration type.
Results:
Sixty-seven patients with 98 NDIs (Premolar site: 81, Molar site: 17, Single crowns: 33, Splinted restorations: 65) were included. The overall implant survival rates were 96.9% at implant level and 97.0% at patient level. Veneer chipping was the most common hardware complication. The veneer chipping rates were 19.4% at patient level and 18.4% at implant level. All patients showed acceptable oral hygiene. Thus, the average MBL was 1.19 mm at implant level and 1.15 mm at patient level. Eight implants (8.5%) and six patients (9.2%) were diagnosed with peri-implantitis. Fifty- eight patients (89.2%) were satisfied with the esthetics of the restorations, while 55 patients (84.6%) were satisfied with the function of the restorations.
Conclusion:
Narrow diameter implants could be a predictable treatment option in the long term. High survival rates, high patient satisfaction, acceptable complication rates and marginal bone loss could be achieved. Further long-term studies are needed to evaluate the predictability of NDIs in molar sites.
KEYWORDS
hardware complication, implant survival, marginal bone loss, narrow diameter implant, patient satisfaction
44 MDI ClinicalStudies from AroundTheUSA
Palm Beach Gardens,Florida 2014
A Literature Review On The Performance Of Narrow- Diameter Implants For Long-Term Overdenture Applications In Maxillary And Mandibular Jaws
2014
Dr.Renee M. Stach
Biomet 3i RESEARCH
Background
The application and popularity of small-diameter implants or “mini-implants” has advanced significantly since they were first introduced to the market in the 1990s. The first “mini-implants” were approximately 1.8mm to 2.0mm in diameter, machined-surfaced and designed so that they could be placed with minimal disruption to the alveolar bone. Their initial intended use were as transitional devices for temporary stabilization of a patient’s immediate prosthesis during the healing phase of submerged standard-diameter implants (SDIs) planned for support of permanent restorations. When used as a transitional device, the mini-implant could provide adequate stability and enhanced mastication while allowing the buried SDIs to osseointegrate during the conventional 4-6 month healing protocol. While mini-implants were generally removed at the end of the transitional period, they were discovered to have osseointegrated to the same extent (bone-to-implant contact) as SDIs [Froum et al. 2005; Zubery et al. 1991]. Due to these findings, the designs and applications of mini-implants have evolved and today they are more commonly referred to as narrow-diameter implants (NDIs), having diameters ranging from 2.2mm to 3.0mm and with surface enhancements to further promote their use as permanent implants. NDIs are appropriate for severely resorbed edentulous regions or narrow ridges, are placed without surgical flap reflection and can be used to support both removable appliances and fixed restorations. When financial considerations play a role in treatment decisions, NDIs are also good options for the edentulous patient.
Objective
The aim of this report is to determine survival rates of narrow-diameter implants placed for long-term stabilization of overdentures in either jaw.
Methods
Literature Search and Strategy
A literature search for journal articles published on clinical studies with outcomes for narrow-diameter implants (NDIs) placed in support of mandibular and/or maxillary overdentures was conducted. Additional inclusion criteria for final selection of studies included the following: NDI diameter ≤ 3.0mm, prospective or retrospective study designs and a follow-up duration ≥ 12 months. Studies needed to provide data on the surgical flap reflection procedure, patient and implant numbers, jaw location, duration of follow-up observations, and cumulative survival rates (CSR). Studies excluded from final selection were those treating patients for transitional overdenture applications or in which data for permanent prostheses could not be separated from overdenture data.
The MEDLINE-indexed database was accessed at the PubMed.gov webpage and literature searches were conducted using the following keywords and combinations: “dental, implant, narrow, small, mini, diameter, mini- implant, overdenture, edentulous”. Search filters included activation of: Humans, Journal type = Dental journals and Search field = Title/Abstract. The search strategy initially focused on selection of systematic reviews for NDIs that would yield the best potential sources of clinical data.
Clinical Data Selection Process
Figure 1 illustrates the selection process for the NDI overdenture clinical studies for this report. The four most recent systematic reviews were selected from the initial literature search: Ortega-Oller et al. 2014*, Klein et al. 2014*, Gleiznys et al. 2012* and Sohrabi et al. 2012*. Each of these articles reviews a distinct number of clinical studies (ranging from 16 to 41) on NDIs of varying diameters and used for different applications. All clinical studies reviewed were between 1995 and 2012. From these articles, clinical studies were selected based on data presented that met
Conclusion
1. NDI systems have transitioned from being used as temporary support devices to long-term stabilization implants.
2. An abundance of long-term clinical data is available to document their utility and performance for overdenture applications in both jaws.
3. Clinical performance rates of NDIs are similar to those of standard-diameter implants.
45 MDI ClinicalStudies from AroundTheWorld
Germany,England 2010
Clinical evaluation of Tiny® 2.5- and 3.0-mm narrow-diameter implants as definitive implants in different clinical situations: a retrospective cohort study. 2010
Anitua E, Errazquin JM, de Pedro J, Barrio P, Begoña L, Orive G.
Eur J Oral Implantol. 2010;3:315-322.
Authors
Anitua E1, Errazquin JM, de Pedro J, Barrio P, Begoña L, Orive G.
eduardoanitua@eduardoanitua.com
Citation
Eur J Oral Implantol. 2010 Winter;3(4):315-22.
Germany,England
Abstract
AIM: The aim of the present study was to assess retrospectively the survival of narrow-diameter implants (2.5 and 3 mm in diameter) in patients with insufficient bone ridge thickness for placement of standard-diameter implants.
MATERIAL AND METHODS:
Fifty-one patients with 89 inserted narrow-diameter implants (2.5 and 3.0 mm) were included. Patients were treated with one or more narrow-diameter implants between June 2004 and December 2005. The observation period for all included implants was at least 3 years after implant loading. Outcome measures were implant survival, complications and marginal bone level changes evaluated on panoramic radiographs.
RESULTS:
The mean follow-up period for all implants was 48 months. Only one implant was lost, yielding survival rates of 98.9% and 98.0% for the implant- and subject-based analyses, respectively. Six complications were reported. Twenty-four months after implant insertion, mean bone loss was 1.26 mm (SD 0.51).
CONCLUSIONS:
Narrow-diameter implants can be successfully used to treat narrow bone ridges up to 3 years after loading.
46 MDI ClinicalStudies from AroundTheUSA
Boston,Massachusetts
Dental Secrets : Third addition. Hanley & Belfus,Inc.
Dr. Stephen T. Sonis,DMD,DMSc
Dept. of Oral Medicine and Diagnostic Services
Harvard School of Dental Medicine.
Q: Do definitive data support the contention that implanted supported teeth should not be splinted to natural teeth?
A: This is controversial,all but available data REFUTE the claim that bridges with both implant and natural tooth abutments do more poorly than bridges supported only by implants.
(Gunne J,Astrand P,Allen K, et al: Implants in partially edentulous patients: A longitudinal study of bridges supported by both implants and natural teeth. Clin Oral Implant Res 3:49-56,1992
47 MDI ClinicalStudies from AroundTheWorld
2010 Egersund Norway.
Long-term outcomes for cross-arch stabilizing bridges in periodontal maintenance patients–a retrospective study.
Fardal O1, Linden GJ.
J Clin Periodontol. 2010 Mar;37(3):299-304. doi: 10.1111/j.1600-051X.2009.01528.x. Epub 2010 Jan 13.
https://www.ncbi.nlm.nih
.gov/pubmed/20070860
Abstract
BACKGROUND:
Cross-arch bridges are used to stabilize teeth for patients with reduced periodontal support. Little is known about technical or biological complications, whether teeth and implants can be combined in this type of bridge and the long-term effects on tooth loss.
MATERIALS AND METHODS:
All patients treated in a specialist periodontal practice who received cross-arch stabilizing bridgework and were subsequently maintained for at least 7 years were included in the study. The patients were selected from all patients who underwent initial periodontal therapy after 1986 in a Norwegian periodontal practice. The bridges were assessed for biological and technical complications. Bridges retained by teeth or by a combination of teeth and implants were included in the study.
RESULTS:
Ninety-four rigid fixed bridges (77 teeth supported, 17 teeth and implant supported) in 80 patients (46 females, 34 males) were observed for an average of 10 years (range 7-22 years). In four patients, a bridge became loose and had to be re-cemented, and in one case the metal framework of a bridge fractured and the bridge had to be remade. In total, eight abutment teeth were lost from five patients but no implant abutments were lost. Overall, a higher rate of tooth loss was observed for patients provided with stabilizing bridges compared with control maintenance patients not treated with bridgework (p<0.0001); however, the rates in both groups were very low.
CONCLUSION:
Cross-arch stabilizing bridges constructed for periodontal patients as part of their periodontal maintenance therapy had few complications and were associated with low rates of abutment tooth loss.
Combining teeth and implants did NOT affect the performance of these bridges.
48 MDI ClinicalStudies from AroundTheUSA.
Lenore,North Coralina
Achieving Success With Small-Diameter Implants
Dentistry Today
2015 Paresh B. Patel, DDS
INTRODUCTION
It is without question that dental implants are one of the most successful additions to modern dentistry. With a success rate of greater than 95%, the root form implant should be considered to restore any edentulous area. However, when we are presented with the need to manage a highly resorbed ridge, significant issues for the surgeon and restorative team arise if only the use of a standard body implant (3.7 mm or larger) is considered. These issues can be anatomical, medical, financial, or restorative.
Anatomical challenges are closely associated with how much residual alveolar ridge remains (quantity) and also its density (quality). These can sometimes be overcome with additional surgical procedures such as ridge expansion, block grafting, and other hard- and soft-tissue procedures. If these solutions are not accepted, the use of a much less invasive procedure should be considered, such as the small-diameter implant (SDI) (also referred to as the mini implant).
SDIs have been around in their FDA-approved form since 1997 and share similar surface texture, coatings, and titanium grade to their larger counterparts. Most implant manufacturers now have added SDIs to their system. These SDIs now are available in one- and 2-piece versions as well as crown and bridge prosthetic options.
Medical challenges should be addressed by utilizing the most minimally invasive surgical plan. The incorporation of 3-D cone beam (CB) technology is rapidly increasing and can allow for presurgical planning to avoid mandatory grafting. A CBCT surgical guide can be created to deliver the implant into the bone with a flapless technique reducing surgical trauma. This may be a prudent solution for patients with systemic conditions who are unable to tolerate lengthy healing times. It is important to note that a CBCT-based surgical guide is much different that a prosthetic guide that is based on a pan x-ray and a stone model.
Restorative challenges are usually the management of restricted restorative space in the mesial-distal or buccal-lingual direction. This has always posed a high-risk problem in the aesthetic area. Too wide of an implant will create potential for bone and/or soft-tissue loss. Convergent roots can also preclude the use of a standard body implant. In these cases, an SDI may allow for the placement of the implant and still allow proper bone support, soft-tissue space, and proper spacing from adjacent tooth roots.
SDIs can be used to retain maxillary or mandibular dentures. Due to reduced surface area, it is recommended to utilize 4 SDIs in the mandible and 6 SDIs in the maxilla. The residual ridge should be of Misch Type I or II to ensure a successful case. If the SDI selected is of a one-piece design, then immediate loading must be addressed. Primary stability should be at a minimum of 30 Ncm on all the implants and a stable tissue supported denture should be delivered. The implants should also be placed as parallel as possible to minimize off-axis loads.
CLOSING COMMENTS
With the use of guided surgery and SDIs, more patients can undergo implant surgery to achieve their desired goals to have teeth. SDIs, along with minimally invasive dentistry, are an ideal treatment solution to consider when standard-body implants are not feasible without additional procedures.
http://www.dentistrytoday.
com/articles/10017
49: MDI ClinicalStudies from AroundTheWorld
Tehran,Iran 2011
Clinical evaluation of small diameter straumann implants in partially edentulous patients: a 5-year retrospective study.
Yaltirik M, et al. J Dent (Tehran). 2011.
Authors
Yaltirik M1, Gökçen-Röhlig B, Ozer S, Evlioglu G.
Author information
1
Associate Professor, Department of Oral Surgery, Faculty of Dentistry, Istanbul University.
Citation
J Dent (Tehran). 2011 Spring;8(2):75-80. Epub 2011 Jun 30.
Abstract
OBJECTIVE: The aim of the present study was to retrospectively evaluate small-diameter (3.3 mm) Straumann® dental implants placed in the maxilla or the mandible over a period of 5 years in function.
MATERIALS AND METHODS: Twenty-eight partially edentulous patients received a total of 48 implants over a 5-year period. After the standard healing period (3 to 6 months),
the implants were restored with single-tooth prostheses or FIXED partial dentures.
All patients were followed according to a strict maintenance program with regular recalls. The cumulative survival rates of implants were analyzed and prosthetic complications were assessed.
RESULTS: After 5 years of function, one single 10-mm-long implant in the maxillary premolar region was lost because of recurrent peri-implant infection in a female patient. Two single 10-mm-long maxillary implants placed in the posterior region were lost due to body fracture. The cumulative 5-year survival rate of the implants was 93.75 %. The most common prosthetic complication was loosening of the occlusal screw.
CONCLUSION: Within the limited observation period and the number of patients included in this study…
it may be concluded that the use of small-diameter implants appears to be predictable if clinical guidelines are followed and appropriate prosthetic restorations are provided.
However, it should be noted that fatigue fracture may occur.
50:MDI ClinicalStudies from AroundTheWorld
Vienna ,Austria 2014
Patients’ preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws.
Review article
Pommer B, et al.
Eur J Oral Implantol. 2014.
Authors
Pommer B, Mailath-Pokorny G, Haas R, Busenlechner D, Fürhauser R, Watzek G.
Academy for Oral Implantology, Vienna, Austria
Citation
Eur J Oral Implantol. 2014 Summer;7 Suppl 2:S91-109.
Abstract
PURPOSE:
To evaluate patient satisfaction, oral health-related quality of life, and patients’ preferences towards minimally invasive treatment options for graftless rehabilitation of complete edentulism by means of dental implants.
MATERIAL AND METHODS:
A MEDLINE search of literature in the English language up to the year 2013 was performed to summarise current evidence from the patient’s perspective. The final selection included 37 studies reporting on minimally invasive implant treatment of 648 edentulous maxillae and 791 edentulous mandibles in 1328 patients, via a total of 5766 implants.
RESULTS:
Patient satisfaction averaged 91% with flapless implant placement (range: 77 to 100%), 89% with short implants, 87% with narrow-diameter implants (range: 80 to 93%), 90% with a reduced number of implants (range: 77 to 100%), 94% with tilted implant placement (range: 58 to 100%), and 83% with zygomatic fixtures (range: 50 to 97%). Indirect comparison yielded patient preference towards tilted implant placement compared to a reduced number of implants (P = 0.036), as well as to zygomatic implants (P = 0.001).
CONCLUSIONS:
While little evidence on patients’ preferences towards minimally invasive treatment alternatives vs. bone augmentation surgery could be identified from within-study comparison,
it may be concluded that patient satisfaction with graftless solutions for implant rehabilitation of completely edentulous jaws is generally high.
Comparative effectiveness research is needed to substantiate their positive appeal to potential implant patients and possible reduction of the indication span for invasive bone graft surgery. PMID 24977244 [Indexed for MEDLINE]
51 MDI ClinicalStudies from AroundTheWorld
Mainz,Germany 2014
Systematic review on success of narrow-diameter dental implants.
Review article
Klein MO, et al. Int J Oral Maxillofac Implants. 2014.
Authors
Klein MO, Schiegnitz E, Al-Nawas B.
Citation
Int J Oral Maxillofac Implants.
rtment of Or al and Maxillofacial Surgery, Plastic Operations, University Medical Center of the Johannes Gutenberg-Universität Mainz, Mainz, Germany.
2Private Practice, Düsseldorf, Germany
2014;29 Suppl:43-54. doi: 10.11607/jomi.2014suppl.g1.3.
Abstract
PURPOSE: The aim of this systematic review was to determine the survival and success rates of narrow-diameter implants (NDI) in different clinical indications compared to standard diameter implants.
MATERIALS AND METHODS: Implant diameters were categorized into categories 1 (< 3.0 mm), 2 (3.00 to 3.25 mm), and 3 (3.30 to 3.50 mm). Retro- and prospective studies with more than 10 patients and a follow-up time of 1 year or more were included.
RESULTS:
A literature search from 1995 to 2012 revealed 10 articles reporting on implant diameters < 3 mm (Category 1), 12 articles reporting on implant diameters 3 to 3.25 mm (Category 2), and 16 articles reporting on implant diameters 3.3 to 3.5 mm (Category 3). The quality of the studies was mostly low with a high risk of bias. Dental implants < 3.0 mm (mini-implants) were one-piece in the edentulous arch and non-loaded frontal region with survival rates between 90.9% and 100%. For dental implants with a diameter between 3.0 and 3.25 mm, most were two-piece implants inserted into narrow tooth gaps without loading and in the frontal region. Survival rates for these implants ranged between 93.8% and 100%. Implants of 3.3 to 3.5 mm were two-piece and were also used in the load-bearing posterior region. Survival rates were between 88.9% and 100%, and success rates ranged between 91.4% and 97.6%. A meta-analysis was conducted for NDI (3.3 to 3.5 mm), which showed no statistically significant difference in implant survival compared to conventional implants with an odds ratio of 1.16 (0.7 to 1.69).
CONCLUSIONS:
Narrow-diameter implants of 3.3 to 3.5 mm are well documented in all indications including load-bearing posterior regions. Smaller implants of 3.0 to 3.25 mm in diameter are well documented only for single-tooth non-load-bearing regions. Mini-implants < 3.0 mm in diameter are only documented for the edentulous arch and single-tooth non-load-bearing regions, and success rates are not available. Long-term follow-up times > 1 year and information on patient specific risk factors (bruxism, restoration type) are also missing. PMID 24660189 [Indexed for MEDLINE]
52:MDI ClinicalStudies from AroundTheUSA
US Utica,NY 2017
Small-Diameter Implants: A 7-Year Retrospective Study.
Brian J. Jackson, DDS
Private practice, Utica, NY
Journal of Oral Implantology
126 Vol. XLIII/No. Two/2017
Oral implantology has become a major discipline within the field of dentistry. Small or mini dental implants have demonstrated success in the retention of removable and fixed prostheses.
Small-diameter implants (SDI) and mini-diameter implants (MDI) describe a group of implants that demonstrate a diameter less than 3 mm.
This retrospective study reports on 335 SDI placed during a 7-year period. All implants were placed in healed sites (.6 months) and loaded immediately or after waiting 3 months. A total of 321 implants were restored and functional within the study’s time interval. A total of 14 implants failed, resulting in a 96.1% implant success rate. Treatment plan considerations should include prosthetic design, specific arch, and immediate load.
Overall, SDI can be utilized as an alternative implant treatment option for patients with atrophic bone, compromised medical histories and financial constraints.
A minimally invasive approach to implant surgical placement has advantages.24
The flapless procedure maintains the periosteum, which distributes the majority of blood flow. Less bone and soft tissue loss is evident.25 A limitation to this approach without a CBCT is a possible error in implant placement. Early failures may be due to implant placement partially in soft tissue.
Small-diameter implant placement leads to reduced osseous compression necrosis leading to enhanced 26 angiogenesis and osteogenesis. The lack of a microgap minimizes surface exposure to pathogenic microorganisms reducing peri-implantitis and subsequent crestal bone loss.27
Implant occlusal principles serve a pivotal aspect for establishing long-term survival rates. A bilateral balanced occlusion exhibiting an anatomical maxillary tooth occluding with a monocline mandibular tooth eliminates interfering excursive movements.28,29 Only 1 implant failed in the fixed prosthesis group, accounting for a high survival rate. The fixed group demonstrated prosthetic concerns of poor esthetics and decementations. The predetermined platform, if exposed after hard and soft tissue healing, can result in an unesthetic result. Modification of the manufactured margin with subsequent traditional impression or intraoral scanning and die fabrication can resolve the problem.
A fixed prosthesis retained by SDI should be designed with narrow occlusal tables, splinted together and cemented with a permanent adhesive.
A resin- modified cement should be utilized for a fixed prosthesis to prevent decementation.30
CONCLUSION
The field of implant dentistry has evolved into a widely accepted dental discipline. Small-diameter implants may be a treatment alternative for some patients. This limited single-site individual private practitioner retrospective study has demonstrated high success rates, suggesting their utilization in specific clinical situations. Small-diameter implant treatment plan considerations should include bone density, prosthetic design, and occlusal factors. Although this retrospective study demonstrates high success rates, additional research focused on SDI is needed prior to wide acceptance by clinicians.
53 MDI ClinicalStudies from AroundTheUSA
Woodstock,NY 2010
Small Diameter Implants
Dr Michael Tischler
DentistryToday/Product Focus
DENTISTRYTODAY.COM • MONTH 2010
Over the past 10 years there has been a definite increase in smaller diameter dental implants on the dental market. In the early 1970’s Dr. Victor Sendax first developed the “mini” implant concept. From that point various companies have evolved to further this “mini” implant market and now there is really 2 groups of these smaller sized dental implants.
Image 1. Small-diameter implant at 1.8 mm to support a mandibular overden- ture.
Image 2. Panograph of 1.8 mm small-diameter implant to support a mandibular overdenture.
Image 3. Panograph of 3 mm one piece small diam- eter implants in function.
Image 4. Periapical radiograph of 3 mm one-piece diameter implant.
Clincial Uses of Small-Diameter Implants
One group can be called the “mini” implant “group” with diameters of 1.8 mm to 2.5 mm and lengths between 10mm to 18 mm. The US Food and Drug Administration (FDA) 510(k) approval for these “mini” implants can be found on the FDA web- site FDA.gov. According to the website the FDA has approved certain brands of dental implants of this size “for use as a self-tapping titanium screw for transitional or intra-bony longterm applications.” They are also indicated according to the FDA web- site for “long-term maxillary and mandibular tissue- supported denture stabilization. Multiple implants should be used and may be restored after a period of time or placed in immediate function.” This is according to the FDA. Another size group of reduced sized dental implants, that are more recently available, can be called the “small diameter implants” This size group is in the 3mm range and to date are all a one piece den- tal implant with the abutment permanently attached. The lengths of these small diameter im- plants are from 12 mm to 18 mm. Dental implants of this size also have FDA 510(k) approval and according to the FDA.gov website. According to the FDA website the 510(k) clearance for 3 mm sized diameter implant is stated as: (1) as an artificial root structure for single tooth replacement of mandibular central and lateral incisors and maxillary lateral incisors. The implant may be immediately restored with a temporary pros- thesis that is not in functional occlusion. (2) when splinted together as an artificial root structure for multiple tooth replacement of mandibular incisors. The implants may be restored after a period of time or placed in immediate function. (3) for denture stabi- lization using multiple implants in the anterior mandible and maxilla. The implants may be restored after a period of time or placed in immediate func- tion. It can certainly be seen that there are approved indicated uses for these sized dental implants. These FDA statements are only guidelines for the dental implants is the reduced cost and adaptability of the prosthesis if an implant were to fail. The literature has shown success with both immediate loading and delayed loading of these smaller sized dental implants. Various attachments are available to secure a denture to the reduced sized implants, and the literature from the available companies will explain the differences. Some clinicians will load the implants immedi- ately, while others will stage the loading of the den- ture. This modality of securing a denture is more cost effective than traditional sized implants and requires minimal available buccal and lingual bone. The cost benefits and the less invasive surgery involved to place these implants, often makes it ideal for the older or medically compromised patient. It is the authors belief that tissue reflection should be utilized for placement of these implants along with adequate radiographic information such as a computed tomography (CT) scan.
TREATMENT PLANNING
FOR A FIXED PROSTHESIS
Treatment planning for reduced sized implants must follow the same guidelines as treatment plan- ning with regular sized implants (3.5 mm to 5 mm width). One advantage of the 3 mm smaller diameter implants, is the ability to place them closer to adja- cent teeth than a regular size implant. The lack of a micro gap between the implant abutment and body allows for this closer proximity according to the lit- erature. This is ideal for their intended use of replac- ing maxillary lateral incisors and mandibular cen- trals and lateral incisors. It is often in these areas that only 5 mm to 6 mm is available between a miss- ing tooth. A CT scan is needed in these situations so that the exact spacing from an axial view can be ascertained. Another reason a CT scan is to avoid excessive angulations and the need to over prep the
Image 1. Small-diameter implant at 1.8 mm to support a mandibular overden- ture.
Image 2. Panograph of 1.8 mm small-diameter implant to support a mandibular overdenture.
Image 3. Panograph of 3 mm one piece small diam- eter implants in function.
Image 4. Periapical radiograph of 3 mm one-piece diameter implant.
Clincial Uses of Small-Diameter Implants
practitioner, and a clinician must make the final deci- sion for their patient. This final decision must be based on correct treatment planning.
TREATMENT PLANNING FOR MINI AND SMALLER SIZED DENTAL IMPLANTS
When treatment planning for any sized dental implants, the principles of loading forces must be taken into account. If a dental implant is overloaded, there is a higher likelihood of bone loss being asso- ciated with the implant and possible failure. The best way to treatment plan for dental implants, is to plan for the placement of dental implants based on the prosthetic end result. These reduced sized dental implants can support both removable and fixed applications. Since these implants have less surface area for the bone to attach to due to their reduced size, the planning for reducing the forces on them becomes even more important.
TREATMENT PLANNING
FOR A REMOVABLE PROSTHESIS:
When utilizing both mini and small diameter implants for a removable denture treatment plan, it must be considered that the implants are not splint- ed and the denture will be primarily tissue support- ed. A clinician should treatment plan for more implants, longer implants, and find the most stable bone possible to reduce loading forces on the implants. These factors will help offset the increased instability of a tissue supported denture with non splinted implants. One advantage of non splinted abutment on the one piece implants.
CONCLUSION
The currently available mini dental implants (1.8 mm to 2.5 mm in width) and small diameter dental implants (3 mm in width) can be used successfully in a variety of clinical situations. It must be emphasized that the reduced surface area of these implants requires correct treatment planning so that loading for- ces do not cause bone loss or implant failure. The reduced costs of treatment for the pa- tient and less invasive sur- gery for placement is an ad- vantage when reduced sized implants support a denture. Another advantage is the prosthetic flexibility if an implant fails. These advan- tages can outweigh the bene- fits of the stability of a bar overdenture on traditional implants for some people. The use of 3mm sized implants are ideal for replacing maxillary lateral incisors and mandibu- lar centrals and laterals. Due to the stringent spacing requirements a CT scan is recommended for placement
54 MDI ClinicalStudies from AroundTheWorld
Willimantic,Conn
Malta 2018
Case report an ectodermal dysplasia patient treated with a small diameter implant supporting a single crown
Aandrea Mascolo,1
Elio Boschetti,1
Dennis Flanagan2
1european Institute for Medical studies, H.e.I. Graduate school, Malta;
2private practice, Willimantic, Ct, Usa
Clinical, Cosmetic and Investigational Dentistry
Dovepress open access to scientific and medical research
https://www.dovepress.com
/getfile.php?fileID=43606
Abstract:
Ectodermal dysplasia (EDD) is a developmental disorder that affects the skin, hair, and teeth among other organs generated in the ectoderm. Dental implants have been used to successfully treat partial edentulism in EDD patients, but the success rate is much lower for these patients. The report herein is a successful case of a single mini, small diameter, implant used to support a single crown of a mandibular right second premolar. A review of implant treatment in EDD patients is included.
Keywords:
dental implant, mini implant, occlusal, load, osseointegration
Introduction
Dental implants can be used to successfully restore partial and complete edentulism. There are patients who present with systemic disorders that may affect outcomes. Ectodermal dysplasia (EDD) is one of these.1,2 There have been reports on successful dental implant treatment in patients with EDD, but the success rate is much lower for EDD patients.3,4 This is a case report of a successful single crown supported by a small diameter, mini, implant in a patient with EDD.
Small diameter implants (SDIs) can be considered for the retention of removable dentures and the support of fixed prostheses especially in narrow ridges. Patients treated with SDIs for removable prosthetic retention had more satisfaction with their rehabilitation than those treated with conventional nonimplant-supported prostheses.30 The treating clinicians reported better retention, masticatory efficiency, and comfort with a positive impact on their QL.3
The low SDI volume of displacement may allow appro- priate healing by not physically blocking angiogenesis and osteogenesis, as well as subsequent bone remodeling.48,49 Nonetheless, the SDI puts a high load on the embedding bone, and the use of a longer SDI may be required to mini- mize the risk of osseous overload.43,48,49 A low cusp height in the occlusal scheme may also lessen the risk of overload of an SDI.43,46
The small percutaneous exposure of SDIs may dramatically reduce the incidence of peri-implant mucositis and peri-implantitis.44 No marginal bone loss was seen with this patient in the postoperative 4 years. Implants may not be appropriate in children who have no complete osseous growth due to drifting and displacement of the bones during maturation.45
Conclusions
SDIs may be a minimally invasive approach for support in fixed prosthetics in selected patients with EDD. Preoperative site evaluation and evaluation of the patient’s disorder and an appropriate occlusal scheme that minimizes off-axial loads is required. This is a case report and is of a low credibility level. In the future, a meta-analysis of case reports and case series may elucidate this topic for appropriate treatment of these individuals.
55 MDI ClinicalStudies from AroundTheWorld
Lenore,NC
Malta 2012
Immediate Load Mini Dental Implant-Supported Zirconia
Crowns by Paresh B. Patel, DDS and Andrea Mascolo, DDS
Dentaltown Magazine
February 2012
Introduction
As implant dentistry becomes more popular, one-piece mini dental implants are increasing in use. There have been several studies that demonstrate that mini dental implants can provide adequate stability for fixed restorations.1 Although considered by some as taboo in mainstream dentistry, the LITERATURE reports SUCCESS RATES SIMILAR to that of conventional implant therapy.2 The purpose of this case report is to challenge traditional thinking and offer patients choices in appropriate situations. All too often patients present to our practices with an inadequate volume of bone for standard size implants (3.75mm).
Dr. Gordon Christensen’s proposed guidelines indicate the need for 6mm of bone in the facial-lingual orientation to accommodate a standard size root form implant.3
To correct these deficiencies and arrive at 6mm of width, additional surgical procedures might be necessary. Some of these patients, who decline additional surgery, would move forward with implant therapy if presented with a viable alternative: the mini dental implant.
This kind of alternative would remove the roadblocks of:
• Bone augmentation (ridge splitting, bone expansion, block grafting)
• Increased expense for the patient
• Increased healing time
• Increased risk of iatrogenic trauma
This case report demonstrates the use of mini dental implants to restore four missing lower incisors in a resorbed residual ridge with four full contour zirconia crowns.
Case Report
The patient, a 70-year-old male, presented for a consultation to replace his missing lower incisors (Fig. 1). The medical history revealed anticoagulation therapy (both Plavix and 81mg aspirin), hypertension and well-controlled diabetes. The survival rates of dental implants in older patients can be affected by certain systemic conditions associated with aging.4 Patients who undergo implant therapy face medical and surgical risks that are similar to those of outpatient oral surgical procedures, regardless of age. The dentist should evaluate the patient for systemic conditions that might compromise healing and the systemic effects of medications.
The lower incisors were lost over a period of time 20 to 25 years ago. His current prosthesis was a cast metal partial that he only wore in social situations. In fact, he called it his “church partial” due to the fact he only wore it when sitting in church with his wife. His desire was to replace the missing incisors with a fixed prosthesis to increase his quality of life, both from a functional and aesthetic perspective. A pan X-ray and study casts were taken for analysis. The lower edentulous area was mapped using the bone-sounding technique as described by Flanagan.5 A severe facial undercut was noted midway down the crest along the entire ridge. A standard size implant would not fit without either reducing the ridge or some bone augmentation, both of which were refused by the patient. This exactly demonstrated why the patient had declined implant therapy seven years ago.
Based off this information, it was decided to utilize four 2.2 x 12mm mini dental implants (OCO Biomedical). The 2.2mm mini implant would allow for bi-cortical stabilization between the facial and lingual plates and provide 1mm of bone to encase the implant in the facial undercut. The mini implants selected have a square prosthetic head to allow for an elegant prosthetic fixed solution. The square prosthetic head is 4.5mm tall to allow the dental laboratory to create a well-fitting restoration.
On the day of placement, the patient was infiltrated in the anterior section with two percent Lidocaine. A pre-operative Peridex rinse was done for 30 seconds along with a single dose of 1,000mg of Amoxicillin one hour prior to implant placement.6
The four sites were marked with a #8 surgical length round bur (Komet) (Fig. 2). A 1.5mm pilot bit from the OCO Mini Implant Kit was used in the externally irrigated implant handpiece (Aseptico) with a drill stop set short of the implant length (Fig. 3). An interesting feature of mini implants is that due to their smaller diameter, the surgical process is greatly simplified. Only one pilot bit is used to take advantage of the self-tapping, bone-condensing design of the mini implant and the visco-elastic property of alveolar bone. The removal of live bone to the diameter of the implant with multiple drills is not necessary. In fact, in most cases with bone mapping, the mini implant can be placed flaplessly, thus preserving the blood supply from the periostium and gingival tissue. This greatly reduces the potential of bone die back as might be expected when making a full flap incision for conventional size implants.
The mini implant is removed from its sterile vile and can be placed by hand with the ultum cap and ratchet wrench or with an implant handpiece driver (Fig. 4). I prefer to place the mini implant with a handpiece for several reasons.
First, the implant motor can be set to 10RPM and 40NCM of torque, thus reducing the potential of overheating the bone from friction or speed of placement.
Second, the use of the implant handpiece prevents lateral torque and creates a true vertical force vector. This ensures a nice tight cortical collar of bone around the mini implant with great primary stability and less potential for micro-movement after surgery. The strong mechanical stability creates osseofixation during the primary phase of bone healing and helps promote osseointegration during the secondary phase over the next eight to 12 weeks. Once all four OCO mini implants were placed to full length, a standard crown and bridge impression was taken with light and heavy body PVS (Capture PVS Glidewell Direct) with the use of the OCO impression snap caps (Figs. 5&6). In this case it was decided to demonstrate the use of an iTero digital impression scanner (Cadent). The mini implants and upper and lower jaws were scanned chairside in the mouth and a virtual model was created (Fig. 7). From this virtual model four individual BruxZir full contour zirconia crowns were fabricated by Glidewell Dental Lab. A resin model was ordered to confirm the fit and contacts (Figs. 8,9a&9b). As more manufacturers are entering the digital impression arena a scan from an IOS FastScan (IOS Technologies) or CEREC (Sirona) could have been used and uploaded via CEREC Connect to create the BruxZir crowns.
I would have rather splinted the four crowns together but it was the patient’s desire to have four individual crowns and the risks associated with not splinting them together were presented at the original appointment.
The patient’s existing partial denture was relieved with a cylinder-shaped acrylic bur (Komet) to fit over the mini implants. At the patient’s seat appointment two weeks later the tissue had already started to climb up the mini dental implants (Fig. 9c). This was a perfect opportunity to utilize a soft-tissue diode laser (AMD Picasso Lite) to remove the overgrowth prior to cementing the crowns. The use of a diode laser allows the clinician to only ablate the target tissue and dramatically minimizes the inflammatory response and bleeding, not to mention that you can touch the implant without fear of disrupting the osseointegration process. PFG gel (Steven’s Pharmacy) was used to anesthetize the tissue for a one-shot appointment. Once the tissue had been recontoured, the aesthetics, fit and occlusion of the zirconia crowns were evaluated. After patient approval, the crowns were cemented with Maxcem Elite resin cement (Kerr Dental) (Figs. 10a&10b). The patient has successfully functioned with the fixed crowns with no complications for one year (Fig. 11).
Discussion
In this case example, the reduced facial-lingual dimension presented a problem for traditional implant therapy. The available bone topography also presented a surgical challenge. With creative but effective treatment planning, a viable solution was presented to attain our patient’s desires. The incorporation of new dental technologies (digital impressions, CAD-milled zirconia restorations and soft-tissue diode lasers) all help to create final products that just a few years ago would have been impossible to offer.
The mini implant can offer advantages in certain situations such as:
• Multiple mini implants can offer adequate surface area needed for successful fixed prosthetics
• Engagement of the cortical plates in thin ridges for excellent primary stabilization.
• One-piece design offers similar strength in a smaller diameter (no screw hole)
• No micro-gap – only radicular and coronal areas in a one-piece design
• Flapless approach to maximize the available blood supply and reduce healing time
• Less volume of bone is removed thus leaving more native tissue to disperse forces
• A pre-contoured abutment that can be shaped in vivo if needed
Conclusion
In a perfect ivory tower practice where time and money are not an issue it would be desirable to replace the missing tissues (hard and soft) to ideal conditions prior to implant therapy. However for most patients, this kind of implant therapy is still unattainable. When possible, patients should be offered traditional implant therapy. With the inclusion of mini dental implants as an alternative, many additional patients can be given a choice other than go home with what they have. It is now up to individual practitioners to become familiar with the vast array of sizes available and the advantages small diameter implants offer.
The problems of ridge deficiency and interden tal space can be solved with the use of mini and small diameter implants. Placement of mini implants (1.8mm-2.4mm) that are retrieved is a well-established procedure used to support fixed or removable prostheses and should be revisited for long-term use.7
With new mini and small diameter implants coming to market almost every day I see a bright future for general dentists willing to get the education they need to offer implant therapy for their patients.
*Dr. Patel reports no conflicts of interest.
References
1 Mini Dental Implants for Long-Term Fixed and Removable Prosthetics: A Retrospective Analysis of 2514 Implants Placed Over a Five Year Period. Todd E Shatkin, DDS, Compendium February 2007;28(2):36-41.
2 Clinical Evaluation of Small-Diameter Implants in Single-Tooth and Multiple-Implant Restorations: A 7-year Retrospective Study, Paolo Vigolo, International Journal of Oral & Maxillofacial Implants.
3 Mini Implants: Good or Bad for Long Term Service?. Gordon Christensen, Journal Compilation 2008 Wiley Periodicals. Volume 20, Number 5. Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failurerates and associated risk factors. Int J Oral Maxillofac Implants 2005;20(4):569-77.
4 Flanagan D. A method for estimating preoperative bone volume for implant surgery. J Oral Implantol. 2000;26:262-266.
5 Journal of Oral and Maxillofacial Surgery in 1997 (The influence of preoperative antibiotics on success of endosseous implants up to and including stage II surgery: a study of 2,641 implants. Dent C, Olson J, Farish S, Bellome J, Casino A, Morris H, Ochi S Journal of Oral and Maxillofacial Surgery December 1997 (Vol. 55, Issue 12 (Supplement), Pages 19-24)).
6 Leshem D, Maxor Z, A simple technique for fabrication of immediate interim removable prosthesis supported by transitional implants. Implant Dent 2003;12:227-231.
56 MDI ClinicalStudies from AroundTheUSA
Buffalo,New York 2017
A Mini Dental Implant Alternative to All-on-Four
DentistryToday
Category: Implants Created:
May 2017
Written by
Brooke Sadkin, and Jared Shatkin
INTRODUCTION
Aesthetic dentistry has evolved throughout the past few decades, specifically in the field of implantology. Patients are preferring endosseous procedures to traditional dentures and other removable prostheses to increase stability and comfort, and to decrease pain.1 Conventional implants require several procedures involving multiple appointments and upwards of a year until completion; although some newer techniques promote a faster completion time. The “All-on-4” technique is an immediate conventional implant procedure in which 4 large-diameter implants (2 in the anterior and 2 in the posterior) are inserted at a 45° angle to take advantage of the available bone and to reduce the need for bone augmentation and/or sinus lift.2 According to Nobel Biocare’s All-on-4 treatment concept manual, a minimum of 5.0 mm in bone width and 8.0 mm in bone height is necessary to begin the procedure.3 (All-On-4 is a registered patent owned by Nobel Biocare developed together with Paulo Malo, DDS, PhD, at the MALO CLINIC.) Though the All-on-4 technique claims to eliminate the need for bone augmentations and sinus lifts, these procedures cannot always be eliminated if the bone quantity does not meet the requirements due to the large diameter of a conventional implant.1-2,4 While the All-on-4 technique offers acceptable support with 4 implants, the endosseous procedure is still invasive and time consuming compared to the immediate and early loading procedures used with mini dental implants. The All-on-4 often requires a minimum of 4 to 6 months before the final restoration is fully completed.4 In addition, if one of the 4 implants fails to integrate or fails following placement of the restoration, the entire restorative procedure must be restarted, additional surgery performed, and the restoration remade. Considering the average fee for All-on-4 is in the range of $30,000 to $40,000 per dental arch, this technique is not affordable for most dental patients.
Technique Using Mini Dental Implants Recently Introduced
Immediate and early loading endosseous procedures with mini dental implants are more desirable to patients in many instances because of the speed of completion, an affordable fee, and it is a less invasive procedure with reduced postoperative discomfort.4 The small size of the mini dental implants (available in several lengths and diameters) eliminates the need for bone augmentation and/or sinus lifts. This is because the mini dental implant can be angled into available bone rather than augmenting the bone.4 The Shatkin Fabricated Implant Restoration and Surgical Technique (F.I.R.S.T.) (patent USPTO No. 7,108,511 B, September 2006; developed by Todd E. Shatkin, DDS) provides for mini dental implant(s) to be placed and restoration(s) cemented in one patient visit.5 The most recent innovation, FIX on SIX (FIX on SIX is a registered trademark owned by Shatkin F.I.R.S.T., developed by Todd E. Shatkin, DDS) offers a combination of the Shatkin F.I.R.S.T. technique using 6 to 8 (or 10) mini dental implants with a 12-unit fixed detachable zirconia full-arch restoration with o-ring implant housings. The restoration is only removed at recall cleanings as the dentist is able to snap off the FIX on SIX restoration. The hygienist will then completely clean the implants, the restoration, and the surrounding tissue and easily reinsert the restoration without patient discomfort. This FIX on SIX procedure is completed in a fraction of the patient’s and the dentist’s time as required by the All-on-4 technique. The success rates of the immediate loading mini dental implant endosseous procedures are competitive with the All-on-4 technique. If one of the mini dental implants were to fail with a FIX on SIX restoration, the failed mini implant can be easily replaced with a new mini implant and o-ring housing placed in the same or different location. In addition, the FIX on SIX restorations are considerably more affordable than the All-on-4 with approximately a 50% to 66% savings. Consequently, the FIX on SIX restorations are more desirable to the patient due to their affordability, greater comfort, reduced treatment time, and the less invasive nature of the procedure.
Figure 1. CBCT Scan from consult
Fixed partial dentures are commonly supported by mini dental implants to provide a natural, aesthetic appearance for the patient. In recent years, zirconium dioxide (zirconia) frameworks have been used in dentistry for fixed restorations.6 The introduction of zirconia has allowed the fabrication of metal-free prostheses via CAD/CAM technology. The result is improved aesthetics with increased success and reliability.7 There is also evidence that there is less plaque accumulation on zirconia, helping to prevent postoperative gingival problems.8 The architecture of these zirconia-based prosthetics enables superior strength and chewing resistance on the posterior teeth relative to other ceramics.5,9 Due to its favorable chemical composition and mechanical properties, clinicians have been eager to use zirconia in implant-supported restorations after its continued success in tooth-supported restorations.10 The following case study (Figures 1 to 15) presents a clinical report of mini dental implants with the FIX on SIX technique. The use of 6 to 8 (or 10) mini dental implants allows for the functional and aesthetically pleasing zirconia fixed prosthesis to be supported. Using CBCT technology, a zirconia prosthetic restoration was created and fixed over Shatkin F.I.R.S.T. mini dental implants (by Intra-Lock) using o-ring housings processed into the zirconia framework.
CASE REPORT
A 56-year-old male patient with an upper denture presented for a consult on May 13, 2016. He had come in after seeing the Shatkin F.I.R.S.T. television marketing campaign. At the consult, our new patient had a CT scan (using our Shatkin F.I.R.S.T. CBCT machine for pre-op and post-op scans) (Figure 1), treatment plan, and impressions taken for a FIX on SIX detachable-removable bridge (Figure 2). To minimize the discomfort and to eliminate the existing issues with his old denture, a zirconia bridge was prescribed and designed to fit on the mini dental implants that would be placed. Zirconia was chosen as the fabrication material due to its strength and durability and resistance to plaque. A treatment plan for placing 10 Mini Drive-Locks (MDL [Intra-Lock]) in the maxillary arch using the Shatkin F.I.R.S.T. technique for mini dental implant placement was chosen. He was asked to return in 2 weeks for his procedure and placement of a temporary bridge.
Figure 2 Model
Fig 3 Thompson marking pen
Fig 4 CT guided stent
Figure 5. Using the Shatkin F.I.R.S.T. Pilot Drill Guide and 20:1 MDL Contra Angle Driver to make Pilot hole
Figure 6. Placing mini dental implant through the CT guided stent with 20:1 handpiece.
Figure 7. Fully seating the mini dental implant after removing the surgical guide stent.
Figure 8. After placing the first 5 mini dental implants, the clinician checks for proper alignment.
Figure 9 The 10 mini dental implants were placed in the maxilla. Notice the bottom of the square is level with the gingiva, and the ball and square are above tissue.
Figure 10. Placing all 10 micro metal housings on the mini dental implants.
Figure 11. Final restoration before placement of o-rings.
Figure 12. Fixed on 10 final restorations with o-rings placed in restoration.
Figure 13. Verification of final zirconia restoration fit
Figure 14. The aesthetics and bite were both checked in the final restoration
Figure 15. Final CBCT and panoramic radiograph
About one month later, the patient returned, signed the consent form, and treatment was begun. A local anesthetic (2 carpules of Septocaine with epinephrine [Septodont]) was administered. A CT guided stent from Shatkin F.I.R.S.T. Lab was used in this case. The position of the 10 implants was marked using a Thompson marking pen and the CT guided stent (Figure 3). Nine Intra-Lock mini dental implants were used on the upper maxillary arch, size 25 mm/15 mm at Nos. 3 to 6 and 9 to 13; and one 25 mm/11 mm for No. 8. The CT-guided stent was used throughout the procedure (Figure 4), removing it between final placement of each implant, using the patented F.I.R.S.T. technique. When finished placing all 10 implants using the Shatkin F.I.R.S.T. procedure, the housings were placed, and A1 Luxatemp (DMG America) was used to create the temporary bridge. The patient liked the temporary. Impressions were taken and sent to the Shatkin F.I.R.S.T. Lab (Figures 5 to 8). Two prescriptions (penicillin 500 mg, Norco 5/325) were sent to the patient’s pharmacy, and an appointment for 2 weeks was made for the delivery of the permanent FIX on SIX detachable-removable bridge. Two weeks later, the patient returned, and the temporary was removed. The FIX on SIX detachable-removable roundhouse restoration was then placed (Figures 9 to 12). The FIX on SIX restoration had good aesthetics, and the patient was happy (Figure 13 to 15). The patient was given a Shatkin Water Flosser and a Sonicare (Philips Oral Healthcare) toothbrush. These are provided as a part of the treatment to our mini implant patients for optimal home care. These have been very successful hygiene tools to keep the soft tissues healthy and clean between checkups, when the FIX on SIX is removed.
CLOSING COMMENTS
This article presents an alternative to All-on-4 that is less expensive, less invasive and painful, and demonstrates faster results while utilizing zirconia, a strong and biocompatible dental material. FIX on SIX is a beautiful zirconia restoration that can be removed by the clinician while providing the patients with the feel and aesthetics of a fixed prosthesis. Creating a fixed prosthesis that is able to withstand the occlusal forces applied, while providing cosmetic appeal and patient satisfaction, is an enduring task for all dentists.11 Today in dentistry, zirconia has traditionally been used in fixed partial dentures as tooth-supported restorations.9,10 With most cases that use zirconia as a fixed restoration, high success rates have been recorded, mostly higher than 95%.9 Zirconia’s ability to increase the durability of a prosthesis by up to 30% to 40% has made it a good candidate for use in fixed-hybrid cases.11 The use of CT technology increases zirconia’s stability in conjunction with decreasing failure rates of these restorations, due to the industrial processing. In this case study, the patient was dissatisfied with his upper denture because of cracks in the acrylic along the palate, and the dentures were not comfortable to wear, and food would trap under them. By designing a fixed zirconia bridge (FIX on SIX) instead of acrylic dentures or a hybrid acrylic fixed bridge, the patient will no longer have these negative experiences. The use of zirconia instead of acrylic increases durability of the prosthesis while also offering the comfort of fixed restoration and healthier surrounding gingival tissues.
References
0. Babbush CA, Kutsko GT, Brokloff J. The All-on-Four immediate function treatment concept with NobelActive implants: a retrospective study. J Oral Implantol. 2011;37:431-445.
0. Jensen OT, Adams MW, Cottam JR, et al. The All-on-4 shelf: maxilla. J Oral Maxillofac Surg. 2010;68:2520-2527.
0. All-on-4 treatment concept [procedures manual]. Kloten, Sweden: Nobel Biocare Services; 2011.
0. Shatkin TE, Petrotto CA. Mini dental implants: a retrospective analysis of 5640 implants placed over a 12-year period. Compend Contin Educ Dent. 2012;33(3, special issue):2-9.
0. Larsson C, Vult von Steyern P, Sunzel B, et al. All-ceramic two- to five-unit implant-supported reconstructions. A randomized, prospective clinical trial. Swed Dent J. 2006;30:45-53.
0. Glauser R, Sailer I, Wohlwend A, et al. Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study. Int J Prosthodont. 2004;17:285-290.
0. Gargari M, Gloria F, Napoli E, et al. Zirconia: cementation of prosthetic restorations. Literature review. Oral Implantol (Rome). 2010;3:25-29.
0. Rimondini L, Cerroni L, Carrassi A, et al. Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants. 2002;17:793-798
0. Komine F, Blatz MB, Matsumura H. Current status of zirconia-based fixed restorations. J Oral Sci. 2010;52:531-539.
0. Guess PC, Att W, Strub JR. Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res. 2012;14:633-645.
0. Cobb GW Jr, Metcalf AM, Parsell D, et al. An alternate treatment method for a fixed-detachable hybrid prosthesis: a clinical report. J Prosthet Dent. 2003;89:239-243.
Dr. Shatkin is a graduate of the University of the Pacific School of Dentistry. He is the president emeritus of the International Academy of Mini Dental Implants and the owner of Shatkin
57 MDI ClinicalStudies from AroundTheUSA
DelrayBeach,Florida 2017
Small-Diameter Implants: Looking Forward
DENTISTRY TODAY ,FEB 2017
Allan Fuhr, DMD
Reflecting back over 40-plus years of practice as an oral sur- geon, I have had the privilege of watching the growth and development of current-day implantology from infancy to today’s contemporary status.
Based on today’s technology and engineering, would you pur- chase a 1998 model car or cell phone or current models?
Easy answer. Why shouldn’t your choice of an implant system be as direct? The “industry” of design, engineering, and manufacturing implants is not stagnant; like that of automobiles and cell phones, it is extremely dynamic. The secret of ongoing success in the prac- tice of implantology is to be aware of and implement the newest technology backed by strategic engineering and science speci c to the brand. Keeping this in mind, we should give some thought to the current small-diameter (mini) implant systems we are currently using in our practices. They certainly deserve our attention because they are surely unique and often play an unsung role in our restorative armamentarium. Throughout the years, we’ve acknowledged and understood the many applications of small-diameter implants but perhaps never gave a second thought to the possibility of a more clinically advanced system.
For stabilizing full and partial dentures as well as assisting in the stabilization of FIXED bridgework, your system seems to do the job.
What You Don’t Know Should Scare You
I remember a manufacturing company that used to tout in its product advertising that “the quality goes in before the name goes on!” How about your small-diameter implant system? Ever research the science or technology associated with the system and/ or manufacturer you are currently using? You may be surprised to hear that there may not be much if anything available.
Figure 1. Mini Drive-Lock instrumentation. Figure 2. OSSEAN surface. Figure 3. Apical end showing BLOSSOM cutting design. DENTISTRY TODAY • FEBRUARY 2017
But don’t be discouraged; there has been some well- founded, documented, publicized infor- mation relative to unique advances in both the technology and science of small-diameter implants and dental implants general. The following information—as uni- versally published in juried scienti c and clinical journals—relates to the technology of Intra-Lock’s implant offerings in particular. A brief synopsis of the journals’ research, technology, and science supported data follows. Additionally, numerous supportive scienti c publications can be found on the website intra-lock.com. Intra-Lock’s Small Diameter Implant Systems, MDL and MILO, were developed more than 15 years ago, and as a result of continuous research and development since then, the company now offers truly advanced systems. Its implants are true “convertible” implants with one-piece solid strength and 2-piece versatility. A choice of implant diameters and lengths provides for varied anatomic challenges. Additionally, a very unique 15° Angled MDL resolves the challenges some- times encountered when placing small-diameter implants in the anterior maxilla.
The company’s patented “Cement-Over Abutments” CONVERT all MDL and MILO Implants from removable to FIXED treatment options.
The systems’ unique Mini Drive-Lock instrumentation (Figure 1) reduces delivery and placement to one fluid motion. All Intra-Lock implants have 2 additional unique and proprietary components. design, is incorporated into the 2.5-mm-diameter MDL and 3.0-mm-diameter Wide Pitch MILO implants.
Unlike traditional tapping designs, BLOSSOM’s architecture enables the implant to cut through bone with increased efficiency and minimal force; hence MINIMIZING BONE compression and micro fracture. BLOSSOM allows for a …LOWER INSERTION TORQUE while decreasing micro movement.
The result: increased initial implant stability. If you are currently using another small-diameter implant system, perhaps your interest in what’s new and exciting has been stimulated. Find some time to do your own research. You owe it to yourself
With 15 years of evolution behind it, the only thing “mini” is the size.
MDL® 15° Implants resolve restorative challenges sometimes encountered in the maxillary anterior region. as a respected dental practitioner, and you certainly owe it to your patients, to offer them your skill and the highest-quality implants that technology and science provide. Remember, the greatest enemy of knowledge is not ignorance; it is the illusion of knowledge. Fighting against illusions in science is a very complex and tricky task, requiring continuing efforts and time. Your approach, in all aspects of implantology, is an important step forward in this endeavor. For more information, call (877) 330- 0338 or visit the website intra-lock.com.
58 MDI ClinicalStudies from AroundTheWorld
Beirut,Lebanon 2015
Use of Narrow-Diameter Implants in the Posterior Jaw:
A Systematic Review.
Assaf, André BDS, DU, MBA; Saad, Moustapha BDS, DU; Daas, Marwan DDS, PhD; Abdallah, Jihad BDS, MScD; Abdallah, Rima BDS, DSc
Implant Dentistry:
April 03, 2015
Basic and Clinical Research:
Abstract
Statement of Problem: Evidence is limited on the efficacy of narrow-diameter implants (NDIs) in the posterior jaw.
Purpose:
The purpose of this systematic review was to assess the survival of NDIs and provide guidelines for their safe use.
Materials and Methods:
Electronic search of the English-language literature enriched by hand search to identify suitable publications was made. Only peer-reviewed clinical studies published from January 1990 through March 2014 were included.
Results:
Seventeen studies with a total of 1644 implants met the inclusion criteria, with an observation period from 1 up to 12 years. The mean survival rate of 98.6% was reported. Technical and other complications were observed.
Conclusion:
Short-term clinical data suggest that NDIs may serve in the posterior jaw as an alternative to standard-diameter implants. However, certain clinical conditions must be observed to assure long-term success.
59 MDI ClinicalStudies from AroundTheWorl d
Mainz,Germany 2014
Systematic review on success of narrow-diameter dental implants.
Review article
Klein MO, et al. Int J Oral Maxillofac Implants. 2014.
Show full citation
Abstract
PURPOSE:
The aim of this systematic review was to determine the survival and success rates of narrow-diameter implants (NDI) in different clinical indications compared to standard diameter implants.
MATERIALS AND METHODS:
Implant diameters were categorized into categories 1 (< 3.0 mm), 2 (3.00 to 3.25 mm), and 3 (3.30 to 3.50 mm). Retro- and prospective studies with more than 10 patients and a follow-up time of 1 year or more were included.
RESULTS:
A literature search from 1995 to 2012 revealed 10 articles reporting on implant diameters < 3 mm (Category 1), 12 articles reporting on implant diameters 3 to 3.25 mm (Category 2), and 16 articles reporting on implant diameters 3.3 to 3.5 mm (Category 3). The quality of the studies was mostly low with a high risk of bias. Dental implants < 3.0 mm (mini-implants) were one-piece in the edentulous arch and non-loaded frontal region with survival rates between 90.9% and 100%. For dental implants with a diameter between 3.0 and 3.25 mm, most were two-piece implants inserted into narrow tooth gaps without loading and in the frontal region. Survival rates for these implants ranged between 93.8% and 100%. Implants of 3.3 to 3.5 mm were two-piece and were also used in the load-bearing posterior region. Survival rates were between 88.9% and 100%, and success rates ranged between 91.4% and 97.6%. A meta-analysis was conducted for NDI (3.3 to 3.5 mm), which showed no statistically significant difference in implant survival compared to conventional implants with an odds ratio of 1.16 (0.7 to 1.69).
CONCLUSIONS:
Narrow-diameter implants of 3.3 to 3.5 mm are well documented in all indications including load-bearing posterior regions. Smaller implants of 3.0 to 3.25 mm in diameter are well documented only for single-tooth non-load-bearing regions. Mini-implants < 3.0 mm in diameter are only documented for the edentulous arch and single-tooth non-load-bearing regions, and success rates are not available. Long-term follow-up times > 1 year and information on patient specific risk factors (bruxism, restoration type) are also missing. PMID 24660189 [PubMed – indexed for MEDLINE]
60 MDI ClinicalStudies from AroundTheWorl d
Ferrara, Italy 2014
Clinical Outcome of Narrow Diameter Implants: A Retrospective Study of 510 Implants
Marco Degidi*, Adriano Piattelli† and Francesco Carinci‡
Correspondence: Dr. Francesco Carinci, Head and Neck Department, Section of Maxillofacial Surgery, University of Ferrara, Corso Giovecca, 203, 44100 Ferrara, Italy. Fax: 39-0532-291582; e-mail: crc@unife.it.
*Dental School, University of Bologna, Bologna, Italy.
†Dental School, University of Chieti, Chieti, Italy.
‡Head and Neck Department, Section of Maxillofacial Surgery, University of Ferrara, Ferrara, Italy.
Journal of Periodontology
Vol. 79: Issue. 1: Pages. 49-54
https://www.ncbi.nlm.nih
.gov/m/pubmed/18166092/
Background:
Narrow diameter implants ([NDIs]; diameter <3.75 mm) are a potential solution for specific clinical situations such as reduced interradicular bone, thin alveolar crest, and replacement of teeth with small cervical diameter. NDIs have been available in clinical practice since the 1990s, but only a few studies have analyzed their clinical outcome.
Methods:
From November 1996 to February 2004, 237 patients were selected, and 510 NDIs were inserted. Implant diameter ranged from 3.0 to 3.5 mm, multiple implant systems were used, and 255 implants were restored immediately without loading (IRWL). No statistical differences were detected among the studied variables. Consequently, marginal bone loss (MBL) was considered an indicator of the success rate (SCR) to evaluate the effect of several host-, surgery-, and implant-related factors. A general linear model (GLM) was used to detect those variables statistically associated with MBL.
Results:
Only three of 510 implants were lost (survival rate [SRR] = 99.4%), and no differences were detected among the studied variables. On the contrary, the GLM showed that delayed loading and longer (>13 mm) and larger (3.4 and 3.5 mm) NDIs reduced MBL.
Conclusions:
NDIs have a high SRR and SCR, SIMILAR to those reported in previous studies of REGULAR DIAMETER IMPLANTS.
Moreover, IRWL of NDIs is a reliable procedure, although a slightly higher bone resorption is reported compared to delayed loading. No implant fractures were detected in the present series.
61: MDI ClinicalStudies from AroundTheWorl d
Valencia,Spain 2013
Narrow-diameter implants: Are they a predictable treatment option?
A literature review
http://www.medicinaoral.com/pubmed/medoralv19_i1_p74.pdf
José-Luis Sierra-Sánchez 1, Amparo Martínez-González 1, Fernando García-Sala Bonmatí 1, José-Félix Mañes- Ferrer 1, Alejandro Brotons-Oliver 2 1 Master in Advanced Oral Implantology Professor, Universidad Europea de Valencia 2 Master in Advanced Oral Implantology Director, Universidad Europea de Valencia
Correspondence:
Clínica Universitaria Odontológica de la Universidad Europea de Valencia C/ Alfambra, 4 – bajo 46009 – Valencia, Spain
joseluis.sierra@uem.es
28/08/2013
Abstract
Objective:
To evaluate the predictability of narrow-diameter implants as a treatment option in routine clinical practice. A literature review was performed of studies reporting clinical results obtained with these implants. Survival rates, peri-implant bone loss and related complications were evaluated. The working hypothesis was that narrow-diameter implants offer clinical results similar to those obtained with implants of greater diameter. Material and Methods: A Medline-PubMed search covering the period between 2002 and 2012 was carried out. Studies published in English and with a follow-up period of at least 12 months were considered for inclusion. A manual search was also conducted in different journals with an important impact factor.
Results:
Twenty-one studies meeting the screening criteria were included in the literature review. A total of 2980 narrow-diameter implants placed in 1607 patients were analyzed.
Conclusions:
The results obtained from the literature indicate that NARROW-DIAMETER IMPLANTS are a PREDICTABLE TREATMENT since they afford clinical RESULTS COMPARABLE to those obtained with implants of GREATER DIAMETER.
62 MDI ClinicalStudies from AroundTheWorld
Zagreb,Croatia 2014
https://hrcak.srce
.hr/file/178865
Initial effects of a treatment by fixed partial dentures supported by mini dental implants from a patient’s point of view. 2014
Authors
Sanja Per{i}1, Antonija Palac2, Denis Vojvodi}1,3 and Asja ^elebi}1,4
1 University of Zagreb, School od Dental Medicine, Department od Prosthodontics, Zagreb, Croatia
2 University of Split, School of Dental Medicine, Department of Prosthodontics, Split, Croatia
3 University of Zagreb, University Hospital Dubrava, Zagreb, Croatia
4 University of Zagreb, University Hospital Centre Zagreb, Zagreb, Croatia
Coll Antropol. 2014 Mar;38(1):275-8.
Abstract
Mini dental implants (MDIs) in dentistry are recommended for cases with adequate bone quality and height, but a lack of alveolar bone width. Some studies well documented successful usage of MDIs for a removable denture support, but studies of MDIs supporting fixed prosthodontic restorations are scarce.
We aimed to study the effect of fixed partial dentures (FPD) therapy supported by MDIs or by MDIs and natural teeth, on patients self perceived oral health related quality of life (OHRQoL), self perceived oral aesthetics and self perceived chewing function. A total of 23 patients (10 female and 13 men, age range from 54 to 78 years) were included and 61 MDIs were inserted, 10 in the maxilla and 51 in the mandible. In 14 patients FPDs were constructed only on MDIs and in 9 patients FPDs were constructed on both, MDIs and natural teeth.
FPDs on MDIs were replacing mostly mandibular incisors, the second maxillary incisors and the first maxillary premolars.
Those FPDs supported by both, MDIs and natural teeth had some MDIs inserted in frontal regions to allow a FPD construction.
The three questionnaires: the OHIP-CRO14 for the assessment of OHRQoL, the OES-CRO for assessment of oral aesthetics and the Chewing function questionnaire (CFQ) for assessment of chewing function have been administrated twice:prior to the MDIs insertion and three months after the FPD treatment supported by MDIs had been finished. The CFQ and the OHIP summary scores significantly decreased revealing better OHRQoL and better chewing ability after treatment, and the OES scores significantly increased indicating increased self perceived oral aesthetics (p < 0.01).
Clinical examination revealed no periimplant inflammation.
Patients’ data supplement the initially promising clinical findings. However, further follow ups will be necessary to finally confirm the long term clinical benefit of MDIs.
63 MDI ClinicalStudies from AroundTheUSA
SanAntonio,Texas
Splinting osseointegrated implants and natural teeth in partially edentulous patients: a systematic review of the literature. 2012
https://www.ncbi.nlm
.nih.gov/pubmed/21073343/
Review article
Mamalis A, et al. J Oral Implantol. 2012.
http://www.joionline.org
/doi/pdf/10.1563/AAID-
JOI
-D-10-00099?download=true
Authors
Mamalis A1, Markopoulou K, Kaloumenos K, Analitis A.
Author information
1
Department of Periodontics, University of Texas, San Antonio, TX, USA. mamalis@uthscsa.edu
Citation
J Oral Implantol. 2012 Aug;38(4):424-34. doi: 10.1563/AAID-JOI-D-10-00099. Epub 2010 Nov 12.
Abstract
Dental implants in partially edentulous patients are a predictable therapeutic option. In patients with reduced bone volume, tooth-to-implant connected prostheses have been described as a treatment option. In this systematic review, the incidence of biologic and technical complications and the long-term survival rates of tooth-implant supported fixed partial dentures (FPDs) are analyzed.
In cases where a natural tooth is connected with an implant to support a FPD, a rigid connection should be preferred.
64 MDI ClinicalStudies from AroundTheWorld
Istanbul,Turkey
Radiographic Evaluation of Narrow-Diameter Implants
After 5 Years of Clinical Function: A Retrospective Study
2013
Onur Geckili, PhD, DDS* Emre Mumcu, PhD, DDS Hakan Bilhan, PhD, DDS
Istanbul University, Faculty of Dentistry, Department of Prosthodontics, ̇Istanbul, Turkey.
Journal of Oral Implantology 275
Journal of Oral Implantology 2013.39:273-279.
http://www.joionline.org/
doi/pdf/10.1563/AAID-JOI
-D-10-00158?code=AAID
-PremDev
The use of regular-sized dental implants is generally recommended to ensure adequate bone to implant contact.
However, when the width of the edentulous crest is insufficient for the placement of a regular-sized implant, the use of a narrow-diameter implant (NDI) should be considered to prevent the need for invasive reconstruction techniques such as grafting procedures.
The aim of the present study was to evaluate the survival and marginal bone levels of NDIs 5 years after prosthetic loading. A total of 159 NDIs belonging to 4 brands (Straumann, Astra Tech, Biolok, Xive) were evaluated in 71 patients. Clinical and radiographic evaluations using digital panoramic radiography were carried out. Two implants failed and no progressive bone loss or periapical lesions were detected in the remaining 157 implants, which is an overall success rate of 98.74%. Mean marginal bone loss (MBL) was found 1 mm on the mesial side and 0.98 mm on the distal side of the implants. No statistically significant relationship was detected between patient age, gender, implant location, implant length, type of the prosthesis, and MBL (P . .05). Among the 4 brands used, the MBL was highest around the Biolok implants but this was significant only compared with the Astra Tech implants (P , .05).
The results of the present study indicate that NDIs can be a good solution for specific clinical situations where regular-sized implants are not suitable.
INTRODUCTION
The dental implant is a very successful tool in the treatment of partial and complete edentulism, making it a popu- lar treatment modality.1,2 In particular cases of single or multiple tooth loss, preparation of healthy teeth adjacent to the edentulous areas is avoided, and the alveolar bone is preserved with implant restorations.3 The use of a wide or regular-sized implant (��4.0 mm) is generally recommended to ensure sufficient bone to implant contact.4–6 However, it should be pointed out that a minimum of 1 mm of bone thickness must surround the entire implant surface.7 1 Istanbul University, Faculty of Dentistry, Department of Prosthodontics, ̇Istanbul, Turkey.
* Corresponding author, e-mail: geckili@istanbul.edu.tr
DOI: 10.1563/AAID-JOI-D-10-00158
In cases of bone atrophy of the long-term edentulous areas or bone loss due to periodontal diseases, periapical pathologies, and traumatic tooth extractions, bone width is usually not adequate for regular-sized implants.8–11 This is because the width of the buccal and lingual bone walls will be diminished and, in particular, the height of the buccal socket wall will be reduced.10,11 Placing a regular-sized implant in such situations may cause large dehiscences, and thus, a risk of complications and failure.7 Moreover, the use of narrow-diameter implants (NDIs) in alveolar bone with a limited buccolingual or mesiodistal width may prevent the risk of injury to neighboring teeth.7,12 To overcome the above mentioned and additional problems related to reduced interdental spaces due to migration or drifting of the remaining teeth, replacement of mandibular incisors and maxillary lateral teeth, and narrow denture-bearing
Evaluation of Narrow Diameter Implants
areas in edentulous patients, almost all implant manufacturers have introduced NDIs (diameter ,3.75 mm).4,13–15 Nevertheless, it has been shown that implants with wider diameters help to reduce maximum stress values in the bone, are mechanically more resistant, and have higher removal torque values than NDIs.16–19 Although NDIs have been available for more than 10 years, few studies have analyzed the clinical outcomes.7,15,16,20,21 These studies mostly showed success rates similar to those of standard-diameter implants. The aim of this retrospective study was to evaluate the survival rate and marginal bone-level changes of NDIs after 5 years of prosthetic loading.
DISCUSSION
This retrospective study analyzed 71 patients with various types of edentulism successfully restored with fixed or removable prostheses supported by 159 NDIs placed by an experienced surgeon at a university clinic. As indicated earlier, all NDIs in this study were placed in alveolar ridges where space limitations prevented the use of wider ones. It should be pointed out that a clarification on nomenclature may need to be addressed by the field of dental implantology concerning mini, narrow, standard, or wide diameter implants. They seem to be blending together in diameter specifi- cations. Although some authors believe an implant with a diameter ,3.75 or 4 mm is narrow or small,13,21–24 others4 think these implants require a minimum mesiodistal space of 6 to 6.5 mm to allow adequate implant to tooth distance and call implants with a diameter ,3 mm NDIs. However, implant designs with diameters below 3 mm have
Journal of Oral Implantology 275
Journal of Oral Implantology 2013.39:273-279.
Evaluation of Narrow Diameter Implants
Table 2
Relationship between the location of narrow-diameter implants (NDIs) and marginal bone loss (MBL)
Location (Mean 6 SD)a
Posterior Maxilla Anterior Maxilla Posterior Mandible Anterior Mandible P
MBL distal 1.01 6 0.26 1.01 6 0.20 0.99 6 0.18 1.00 6 0.19 .956 MBL mesial 0.98 6 0.26 0.98 6 0.21 0.99 6 0.18 0.96 6 0.17 .925
a One-way analysis of variance.
been introduced into the market under the banner of ”mini implants.”25,26 In a few published studies, small- or narrow-diameter implants were classified in a specific dimension range.7,20 Comfort et al20 regarded implants of 3.0–3.3 mm in diameter as small; whereas implants with a diameter of 3.0 to 3.4 mm were called narrow by Davarpanah et al.7 In all of these studies, implants with a diameter of 3.75 or 4.0 mm were regarded as regular-sized implants. The implants that we evaluated were 3.3 to 3.5 in diameter and were all below the regular size; thus, calling them narrow was deemed appropriate in the present study.
As the smaller-diameter implants known as mini implants25,26 were not used in this study, the results cannot be applied to these mini implants.
The overall implant success rate after 5 years of loading time (98.74%) indicated that NDIs can be successfully used to support fixed or removable prosthesis. This implant success rate is consistent with previous studies investigating the outcome of NDIs.16,20–23 Orthopantomography is a reliable radiographic procedure, and because of its standardized projec- tion in the vertical plane, it is well suited for vertical measurements.24,27,28 It has been shown that panoramic radiographs provide trustworthy infor- mation to assess the point of bone attachment to implant threads.29 Although the best methods in bone measurements are considered to be dental volumetric tomography or subtraction radiography using standardized periapical radiographs, it should be pointed out that in routine practice these techniques are too impractical and present difficul- ties for patients.24,27–30 For standardized periapical radiographs, a custom-made film holder must be developed and mounted on the implant to ensure standardized exposure. Additionally, for the correct performance, the restoration and abutment must be unscrewed from the implant, which is a process patients usually do not prefer. Also, uncomfortable film holders are usually very painful for patients with atrophic mandibles.30 Panoramic radiographs are a practical alternative to periapical radiographs for evaluating MBL in cases where this type of edentulous mandible makes intraoral periapical radiography difficult or impossible.27,28,30 Further- more, computer-aided panoramic radiography, which was used in the present study, has been confirmed to provide accurate and repeatable measurements with the help of calibration using the known implant dimensions in a similar study investigating the clinical and radiographic outcome of NDIs.21 Most of the previously published studies dealing with the MBL of implants agree that neither age nor gender of patients seem to be an important factor on peri-implant bone loss, which supports the present findings.3,29 Based on previous assumptions, it is widely accepted that MBL of 1 mm during the first year after prosthetic loading, and an annual bone loss not exceeding 0.2 mm thereafter is a natural feature and consistent with successful treatment.2,29,31,32 The mean MBL found in the present study (1.0 mm at the mesial side and 0.98 mm at the distal side of the implants) satisfies these assumptions. Because this was a retrospective study investigating the MBL of NDIs 5 years after prosthetic loading, it was not possible to monitor the marginal bone level changes 1 year after prosthetic loading, which is a limitation of this study. Nevertheless, it is assumed that the major part of the MBL may have occurred during the first year after prosthetic loading; thereafter, the marginal bone levels stabilized. The survival rate and bone levels found were similar to those found in previous studies of regular-sized implants.33–40 However, this result is not in accor- dance with previous experimental findings using finite-element analyses in which reduced stress and strain patterns were observed with wider diameters as a result of increased bone to implant contact
276 Vol. XXXIX/Special Issue/2013
Journal of Oral Implantology 2013.39:273-279.
Downloaded from
Geckili et al
Table 3
Comparison of implant brands in terms of marginal bone loss (MBL)
Implant Brands (Mean 6 SD)a
Implant A Implant B Implant C Implant D
(Straumann; n 1⁄4 49) (Astra Tech; n 1⁄4 42) (Biolok; n 1⁄4 37) (Xive; n 1⁄4 31) P
MBL distal 0.99 6 0.23 0.94 6 0.21 1.09 6 0.18 1.01 6 0.19 .019* MBL mesial 0.96 6 0.23 0.93 6 0.20 1.06 6 0.19 0.99 6 0.16 .040*
a One-way analysis of variance. *P , .05.
area; the researchers concluded that this reduction
would in turn result in less MBL around the neck of implants.6,17,18,41
The lowest MBL rate, which was also significantly lower than the MBL of implant C, was observed in implant B in the present study. The superiority implant B for MBL was similarly reported in other clinical studies comparing the MBL of different brands.42–44 It seems that the differences in surface texture and shape of the implant neck between the implant systems result in significant differences in the magnitude of MBL. However, it should be noted that since the present study was retrospective, there was no randomization of implants and there was an unequal distribution of implants among the 4 brands used. Therefore, further randomized controlled clinical trials comparing different brands of NDIs are needed to draw more reliable conclu- sions. Reducing the diameter of the implants was shown to increase the risk of fractures due to lower mechanical durability.45,46 Fatigue fracture may occur in NDIs after a long period of function.22,46 In 2 long-term studies, the fracture rate of NDIs was reported to be around 0.67% and 0.26%, respec- tively.22,23 The NDIs followed for 5 years in the present study showed no signs of fractures. This result could be because the NDIs were splinted with each other or to other regular-sized implants when possible, which was consistent with the results of 2 similar studies.20,21 Although a previous study pointed out that compression/tension forces were lower in the overdenture situations than with a fixed prosthe- sis,47 the type of prosthesis, whether a fixed or removable denture, did not influence the MBL rates in the present study. As there was an unequal distribution of prosthesis type, it is not possible to make an exact conclusion on this subject. Survival and MBL of NDIs does not seem to be affected by implant location, according to the results of the present study. However, because of the low number of implant failures observed in the current study, it was not possible to confirm these results. Previous studies have shown that NDIs of shorter lengths, such as 7 or 8 mm, fail disproportionally in comparison with implants of 10 mm or longer.33,34 No relationship was found between implant length and MBL in the present study, which is in accordance with previously published studies.20,21 All the implants used in the present study were 11 mm or longer. Therefore, it was not possible to monitor the marginal bone level changes of shorter NDIs, which can also be regarded as another limitation of this study.
CONCLUSION
Within the limitations of this study, it can be concluded that survival and MBL rates of NDIs seem to be comparable with those of regular-sized implants and that NDIs can be used confidently when anatomic situations do not permit the use of wider ones.
65 MDI ClinicalStudies from AroundTheWorld
Vancouver,Canada
A Literature Review On The Performance Of Narrow-Diameter Implants For Long-Term Overdenture Applications In Maxillary And Mandibular Jaws 2014
Renée M. Stach†, DDS
†Dr. Renée Stach is an employee of BIOMET 3i LLC.
Background
The application and popularity of small-diameter implants or “mini-implants” has advanced significantly since they were first introduced to the market in the 1990s. The first “mini-implants” were approximately 1.8mm to 2.0mm in diameter, machined-surfaced and designed so that they could be placed with minimal disruption to the alveolar bone. Their initial intended use were as transitional devices for temporary stabilization of a patient’s immediate prosthesis during the healing phase of submerged standard-diameter implants (SDIs) planned for support of permanent restorations. When used as a transitional device, the mini-implant could provide adequate stability and enhanced mastication while allowing the buried SDIs to osseointegrate during the conventional 4-6 month healing protocol. While mini-implants were generally removed at the end of the transitional period, they were discovered to have osseointegrated to the same extent (bone-to-implant contact) as SDIs [Froum et al. 2005; Zubery et al. 1991]. Due to these findings, the designs and applications of mini-implants have evolved and today they are more commonly referred to as narrow-diameter implants (NDIs), having diameters ranging from 2.2mm to 3.0mm and with surface enhancements to further promote their use as permanent implants. NDIs are appropriate for severely resorbed edentulous regions or narrow ridges, are placed without surgical flap reflection and can be used to support both removable appliances and fixed restorations. When financial considerations play a role in treatment decisions, NDIs are also good options for the edentulous patient.
Objective
The aim of this report is to determine survival rates of narrow-diameter implants placed for long-term stabilization of overdentures in either jaw.m
Methods
Literature Search and Strategy
A literature search for journal articles published on clinical studies with outcomes for narrow-diameter implants (NDIs) placed in support of mandibular and/or maxillary overdentures was conducted. Additional inclusion criteria for final selection of studies included the following: NDI diameter ≤ 3.0mm, prospective or retrospective study designs and a follow-up duration ≥ 12 months. Studies needed to provide data on the surgical flap reflection procedure, patient and implant numbers, jaw location, duration of follow-up observations, and cumulative survival rates (CSR). Studies excluded from final selection were those treating patients for transitional overdenture applications or in which data for permanent prostheses could not be separated from overdenture data. The MEDLINE-indexed database was accessed at the PubMed.gov webpage and literature searches were conducted using the following keywords and combinations: “dental, implant, narrow, small, mini, diameter, mini- implant, overdenture, edentulous”. Search filters included activation of: Humans, Journal type = Dental journals and Search field = Title/Abstract. The search strategy initially focused on selection of systematic reviews for NDIs that would yield the best potential sources of clinical data. Clinical Data Selection Process Figure 1 illustrates the selection process for the NDI overdenture clinical studies for this report. The four most recent systematic reviews were selected from the initial literature search: Ortega-Oller et al. 2014*, Klein et al. 2014*, Gleiznys et al. 2012* and Sohrabi et al. 2012*. Each of these articles reviews a distinct number of clinical studies (ranging from 16 to 41) on NDIs of varying diameters and used for different applications. All clinical studies reviewed were between 1995 and 2012. From these articles, clinical studies were selected based on data presented that met *BIOMET 3i Implant clinical data was included in some of the studies reviewed by these authors as well as the PubMed search. However, BIOMET 3i did not provide any financial support for the systematic reviews.
Conclusion
1. NDI systems have transitioned from being used as temporary support devices to long-term stabilization implants.
2. An abundance of long-term clinical data is available to document their utility and performance for overdenture applications in both jaws.
3. Clinical performance rates of NDIs are similar to those of standard-diameter implants.
*The following retrospective studies were excluded due to the lack of specificity on critical data: Bulard & Vance 2005, LaBarre et al2008, and Shatkin & Petrotto 2012.
References
Anitua E, Errazquin JM, de Pedro J, Barrio P, Begoña L, Orive G. Clinical evaluation of Tiny® 2.5- and 3.0-mm narrow-diameter implants as definitive implants in different clinical situations: a retrospective cohort study. Eur J Oral Implantol. 2010;3:315-322.
Anitua E, Orive G, Aguirre JJ, Ardanza B, Andía I. 5-year clinical experience with BTI dental implants: risk factors for implant failure. J Clin Periodontal. 2008;35:724-732.
Bulard RA, Vance JB. Multi-clinic evaluation using mini-dental implants for long-term denture stabilization: a preliminary biometric evaluation. Compend Contin Educ Dent. 2005;26:892-897.
Cho SC, Froum S, Tai CH, Cho YS, Elian N, Tarnow DP. Immediate loading of narrow-diameter implants with overdentures in severely atrophic mandibles. Pract Proced Aesthet Dent. 2007;19:167-174.
Elsyad MA, Gebreel AA, Fouad MM, Elshoukouki AH. The clinical and radiographic outcome of immediately loaded mini implants supporting a mandibular overdenture. A 3-year prospective study. J Oral Rehabil. 2011;38:827-834.
Froum SJ, Simon H, Cho SC, Elian N, Rohrer MD, Tarnow DP. Histologic evaluation of bone-implant contact of immediately loaded transitional implants after 6 to 27 months. Int J Oral Maxillofac Implants. 2005;20:54-60.
Gleiznys A, Skirbutis G, Harb A, Barzdziukaite I, Grinyte I. New approach towards mini dental implants and small-diameter implants: an option for long-term prostheses. Stomatologija. 2012;14:39-45.*
Griffitts TM, Collins CP, Collins PC. Mini dental implants: an adjunct for retention, stability and comfort for the edentulous patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:e81-84.
Jofré J, Cendoya P, Munoz P. Effect of splinting mini-implants on marginal bone loss: a biomechanical model and clinical randomized study with mandibular overdentures. Int J Oral Maxillofac Implants. 2010;25:1137-1144.
Klein MO, Schiegnitz E, Al-Nawas B. Systematic review on success of narrow-diameter dental implants. Int J Oral Maxillofac Implants. 2014;29 Suppl:43-54.*
LaBarre EE, Ahlstrom RH, Noble WH. Narrow diameter implants for mandibular denture retention. J Calif Dent Assoc. 2008;36:283-286.
Maryod WH, Ali SM, Shawky AF. Immediate versus early loading of mini- implants supporting mandibular overdentures: a preliminary 3-year clinical outcome report. Int J Prosthodont. 2014;27:553-560.
Morneburg TR, Pröschel PA. Success rates of microimplants in edentulous patients with residual ridge resorption. Int J Oral Maxillofac Implants. 2008;23:270-276.
Mundt T, Schwahn C, Stark T, Biffar R. Clinical response of edentulous people treated with mini dental implants in nine dental practices. Gerodontology. 2013 Jul 17.[Epub ahead of print]
Ortega-Oller I, Suárez F, Galindo-Moreno P, Torrecillas-Martínez L, Monje A, Catena A, Wang HL. The influence of implant diameter on its survival: a meta-analysis based on prospective clinical trials. J Periodontal. 2014;85:569-580.*
Preoteasa E, Imre M, Preoteasa CT. A 3-year follow-up study of overdentures retained by mini-dental implants. Int J Oral Maxillofac Implants. 2014;29:1170-1176.
Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17 Suppl 2:35-51.
Shatkin TE, Petrotto CA. Mini dental implants: a retrospective analysis of 5640 implants placed over a 12-year period. Compend Contin Educ Dent. 2012;33 Spec 3:2-9.
Sohrabi K, Mushantat A, Esfandiari S, Feine J. How successful are small-diameter implants? A literature review. Clin Oral Implants Res. 2012;23:515-525.*
Zubery Y, Bichacho N, Moses O, Tal H. Immediate loading of modular transitional implants: a histologic and histomorphometric study in dogs. Int J Periodontics Restorative Dent. 1999;19:343-353.
*BIOMET 3i Implant clinical data was included in some of the studies reviewed by these authors as well as the PubMed search. However, BIOMET 3i did not provide any financial support for the systematic reviews.
**Studies which included BIOMET 3i Implants did not meet the inclusion criteria for this literature review and were excluded in the selection process. BIOMET 3i Implants are not part of the clinical data examined in this paper.
3M is a trademark of 3M Co. and ESPE is a trademark of 3M ESPE. Brasseler USA is a registered trademark of Brasseler USA. BTI is a registered trademark of BTI of North America. Frialoc is a registered trademark of DENSPLY Implants. Southern Implants is a registered trademark of Southern Implants Inc. SteriOss and TiUnite are registered trademarks of NobelCare. Providing Solutions – One Patient At A Time is a trademark of BIOMET 3i LLC. LOCATOR is a registered trademark of Zest Anchors, Inc. ©2015 BIOMET 3i LLC. All trademarks herein are the property of BIOMET 3i LLC unless otherwise indicated. This material is intended for clinicians only and is NOT intended for patient distribution. This material is not to be redistributed, duplicated or disclosed without the express written consent of BIOMET 3i. For additional product information, including indications, contraindications, warnings, precautions and potential adverse effects, please visit the BIOMET 3i Website: www.ifu.biomet3i.com. ART1269 REV A 03/15
66 MDI ClinicalStudies from AroundTheUSA
Meridian,Ohio 2017
Past,Present,& Future of Narrow Diameter Implants
Dr. Terra Greene
Meridian,Idaho
Abstract
Narrow diameter implants, mini-implants, small diameter implants, category 1 implants—whatever you choose to call implants defined as less than 3.0 mm in diameter—have been cleared by the Food and Drug Administration for a considerable period of time. They are indicated for several treatment modalities, including FIXED PROSTHESIS, removable complete dentures, and temporization.
They have been found to improve treatment acceptance, particularly where anatomical, financial, and/or medical challenges are present that otherwise impede conven- tional implant treatment.
There is a crucial gap between the numbers of patients who would benefit from implant treatment and the number of procedures that are performed.
According to the American College of Prosthodontists, 178 million people in the United States are missing at least one tooth. And yet only 2.3 million implant- supported crowns are made annually.1
Implant Breakthrough
In the early 1990s, Bernard Weissman understood why so many implant treatment plans did not receive case acceptance and summarized it in terms of time, bone, money, and fear of surgery. This drove him to develop the first narrow diameter implant that was 1.8 mm in diameter. It was a one-piece, self- threading implant designed for transitional use that would be placed at the same time of stage-one implant surgery, and was immediately loaded so that (1) patients never had to be without teeth, and (2) surgical sites would remain completely protected. This was an amazing breakthrough. Questions then arose. How long would these narrow diameter implants last? Would they actually osseointegrate? Those ques- tions were answered in 2004 when the FDA approved narrow di- ameter implants for “long-term use and for any length of time as decided by the health-care provider.”2 Further, Dr. Stuart Froum, clinical professor and director of clinical research, Department of Periodontology and Implant Dentistry, New York University Dental Center, along with Dr. Michael Rohrer, Professor and Director of the Hard Tissue Research Laboratory, School of Dentistry, University of Minnesota, Department of Diagnostic and Biological Sciences, Division of Oral and Maxillofacial Pathol- ogy, et al. published a histology report concluding that “the percentage of bone to implant contact achieved with these implants was similar to that documented in the literature for conventional turned, screw-shaped, machine-surfaced implants.”3 The percentage of BIC achieved was similiar to that documneted in the literature for conventional turned, machine-surface implants Histology of Dentatus Narrow Diameter Implants Calls For Action In November 2004, the American Dental Education Association (ADEA) called a special meeting of deans and industry representatives to review the status of implant dentistry in the curriculum. Two initiatives resulted from this meeting: (1) a call for use of a single implant to replace the three-unit bridge and prevent cutting virgin teeth, and (2) a two-implant overdenture should become the first choice of treatment for the edentulous mandible.4
The McGill Consensus statement reported overwhelming evidence in support of the two-implant overdenture.5
Jung, Lang, et al. deemed an implant-supported crown the evidence-based option of choice for replacement of a single anterior tooth with adjacent virgin teeth neighbors in an otherwise sound dentition.6 And yet, today there are still barriers to these levels of care. In order to increase implant treatment acceptance, Dr. Avishai Sadan, former editor in chief of Quintessence International, urged dentists to focus on objective data rather than descriptive terms. “Patients described how the treatment plan for a three-unit fixed partial denture versus a single implant restoration was presented: ‘You are missing a tooth and it needs replacement. We can file down the teeth adjacent to the miss- ing tooth and give you the bridge in about four weeks. Alternatively, we can drill a hole in your jaw, put a screw in there, and put a crown on that. This approach will take about a year.’ Even patients who did not want their teeth prepared for a fixed partial denture opted for that treatment plan because the hole in the head alternative was less appealing.”7
It is well documented and generally accepted today that if a tooth is missing, an implant is the option of choice.
Just as important as the language we select in treatment presentation is the ability to offer multiple solutions within the field of implantology. The end goal is the same: we want our patients to benefit from the numerous advantages of implants with regard to function and preservation of bone and esthetics, irrespective of size or brand.
Many times narrow diameter implants can overcome patient objections because they address specific, and often overlapping, well-known concerns.
They offer a minimally invasive, affordable solution that is within reach for most patients. They eliminate the need for a two-stage surgery and having to wait for their teeth. Another advantage of the narrow diameter implant is that flap surgery is often unnecessary and sutures are not needed.8
Turning Point
The right combination of factors—both TECHNICAL and ECONOMICAL , among others—align to shift a product from that of a luxury to an EVERYDAY ITEM.
Today, the adoption of new products is happening at an increasingly rapid pace. Considering dental implants in this context, the trend toward this treatment becoming commonplace is clear. We see medical practices redefining their roles. They are recognizing a broader societal responsibility to acknowledge the real value of health-care expenses and the treatment results. Thus, medical doctors are urged to consider the economic consequences of their decisions.9
Likewise, in dentistry, we recognize that a one-size-fits-all approach to implantology is no longer viable.
Textbook dentistry—the gold-standard, top-of-the-line, A-one treatment plans—must adapt to circumstances to meet the needs of a larger patient population.
The BENEFITS of NARROW DIAMETER implants offer one such solution to overcoming obstacles relating to clinical, medical, emotional, and/or financial means.
Today, we see NUMEROUS AUTHORS reporting SUCCESSFUL RESULTS when narrow diameter implants were used to support definitive prostheses.10-14 Bidra and Almas reported a 94.7% SURVIVAL RATE of narrow diameter implants when used exclusively for definitive prosthodontic treatment in a systematic review of literature in 2013.15
Sohrabi et al. also conducted a literature review and concluded “no significant difference in failure and complication rates between narrow body implants and standard-diameter implants.” 16
Had a survival rate comparable to standard-diameter implants
Displayed an annual bone loss comparable to standard-diameter implants.
Achieved favorable esthetic results 21
Research shows that when used appropriately, narrow diameter implants offer a PRACTICAL practical and PEEpredictable solution.
As best explained by Dr. Dennis Tarnow, clinical professor of periodontology and director of implant education at Columbia School of Dental Medicine, “The bone does not know the dif- ference between a 1 mm implant or a 9 mm implant. What mat- ters is what you do on top of it.”17 Since their inception, narrow diameter implants—classified here as under 3.0 mm in diameter—have undergone advances in material (grade V Ti-alloy), surface (treated to increase surface area and improve osseointegration), and prosthetic design (screw-retained with abutment variety comparable to conventional implants), all working to improve the ease of use and success rates. Increasing Access to Care As it stands today, of the patient population that actually goes to the dentist, only 10% of those that could benefit from an implant actually proceed with treatment.18-20 According to the American Academy of Implant Dentistry (AAID), the dental implant and prosthetic market in the US is projected to reach $6.4 billion by 2018—a $6.4 billion-dollar industry fueled by 10% of the population.20 In order to maxi- mize profits, a conventional implant company needs to add to their product offerings. We see that happening with the likes of grafting materials, new membranes, and the advent of digital dentistry, all of which are amazing advances making implan- tology more predictable and successful. But those advances add cost to the procedure and fail to address the 90% who go without treatment. Narrow diameter implants are particularly effective where anatomical, financial, and medical challenges are present that otherwise impede conventional implant treatment.
Increasing Treatment Options
Because they require less overall intervention, often eliminate the need for bone grafting procedures, and greatly reduce the number of chairside visits, narrow diameter implants are quickly being recognized as one of the best additions to the armamentarium for dentists to treat patients who are missing one tooth or more. The high success rate of implants has also expanded treatment options for both dentists and patients. Primarily, narrow diameter implants can be placed into anatomically challenging areas that would be contraindicated for standard diameter implants without site modification procedures—procedures that add to treatment time, overall cost, and morbidity, all of which can deter patients from dental implant therapy.
Advantages of Narrow Diameter Implants
Eliminate grafting
Often flapless technique
Immediately loaded restoration
Reduced chair time / number of visits
Cost effective
No preparation of adjacent teeth
Retrievability
Narrow Spaces
In areas of limited bone width, limited mesial-distal space, or converging roots, narrow diameter implants are an ideal solu- tion. A narrow diameter implant makes it possible to maintain adequate bone dimensions and proper implant spacing without augmentation, as well as preserving the buccal plate, because less bone is prepared for the osteotomy. The tapered design facilitates the one-stage surgery and is more conducive to a minimally in- vasive, flapless implant placement. This eliminates many post- operative challenges and decreases patient post-op discomfort. Narrow diameter implants avoid the need for preparation and/or reduction to the adjacent natural dentition. They al- low patients who normally would have to proceed with a fixed bridge or resin-bonded bridge the option of dental implants. These patients include those with congenitally missing incisors, reduced interdental space following orthodontic move- ment, one or two missing mandibular incisors, or space collapse in the maxillary anterior area where orthodontic work was not considered a viable option. A screw-retained abutment offers many prosthetic options and affords more flexibility for long-term maintenance. The restoration is retrievable and thus allows for repair or recoloring of the crown.
In a 14-year retrospective case series, Dr. Froum et al. reported an ANNUAL BONE LOSS of <0.02 mm on narrow diameter implants, which is CONSIDERABLE LESS than that typically reported for STANDARD DIAMETER IMPLANTS (.22-.80mm) 21 due in part to the SOLID,ONE-PIECE implant design that ELIMINATES the MICROGAP , REDUCING CRESTAL BONE LOSS.
Overdentures
An implant-retained denture can sometimes be considered the preferred treatment method, as it can provide support in cases of facial collapse. Numerous authors show successful results us- ing two to four implants to retain an overdenture, both in terms of implant survival and patient satisfaction.22-27 But oftentimes, anatomic limitations and resorbed ridges compromise the num- ber of implants, length, and position.28 Narrow diameter implant protocol recommends that four implants be placed between mental foramina, offering stabilization and cross-arch support and preventing rocking often seen with two-implant techniques. In elderly patients with advanced medical issues or on antico- agulant therapy, the placement of more than one implant has been shown to have a statistically increased risk of complication.29 Nar- row diameter implants simplify the procedure for patients who are not candidates for conventional implants—a minimally invasive flapless surgery without bone augmentation results in little post- op bleeding and decreased pain. Narrow diameter implants also preserve the jaw structure, preventing atrophy from bone loss. A University of Gothenburg study on narrow diameter im- plants for overdenture retention by Tomasi et al. noted positive patient-centered outcomes of 100% satisfaction and reduced treatment times for patients presenting with compromised health conditions (61%) and not in a condition to receive conventional implant surgical treatment. For the other patients, economic restrictions (29%) and fear of surgical treatment (10%) were rea- sons to opt for narrow diameter implant treatment rather than conventional surgery.30 Temporization When narrow diameter implants are not considered for a long-term solution, they still present a valuable modality in supporting fixed provisional restorations. At times when bone grafting is necessary to place and restore an implant, narrow diameter implants can protect the augmented site with a fixed provisional restoration, offering a comfortable and acceptable solution as compared to a removable denture. Narrow diameter implants allow a patient to undergo lengthy treatments without ever losing function or suffering the embarrassment of having to go without teeth. In some instances, the implants intended for provisionaliza- tion can be incorporated into the definitive prosthesis as well. In a case study with 11-year follow up, Froum, Misch, et al. found that “these implants achieve excellent osseointegration and may be used long term to support the definitive prosthesis when splinted to standard diameter implants.”31 Areas of Use Single-tooth restorations Congenitally missing laterals, converging roots, limited interdental space Multi-unit bridges Thin ridges Immediate temporization Protection of grafted sites, surgical guide stabilization, tissue architecture Overdenture retention Can later be converted to fixed restoration with Elypse coping 4
www.DentalAcademyOfCE.com
Case Studies
Limited interdental spaces
Case courtesy of Dr. Paul Petrungaro, periodontist, Chicago, IL. Case originally appeared in Inside Dentistry, March 2006.
A 14-year-old nonsmoking girl presented for replacement of the congenitally missing right lateral incisor (tooth No. 7). The patient’s orthodontic treatment had resulted in a compromised implant receptor site. Along with her parents, the patient refused any reduction of the virgin natural teeth, and did not accept the option of a resin-bonded bridge. The use of a removable prosthe- sis was contraindicated because of the patient’s significant gag reflex. At the gingival level, the edentulous space measured 4.7 mm from the mesial of tooth No. 6 to the distal of tooth No. 8. Conventional implant dimensions were unacceptable to treat this compromised edentulous space. For these reasons, the Dentatus ANEW 2.4-mm x 14-mm implant was selected for placement, and the immediate provisionalization procedure was selected to allow the patient to have a nonremovable tooth option.
5. 6.
1. Preoperative view of the maxillary right lateral incisor space
2. Preoperative periapical radiograph
3. Placement of the Dentatus ANEWTM implant
4. The completed provisional restoration
5. The final implant-supported restoration
6. The digital periapical radiograph of the completed case
Long-term in patients unable to receive conventional implants
Case courtesy of Tommaso Ravasini, DMD, Parma, Italy. Case originally appeared in Inside Dentistry, Jul/Aug 2007.
A distraught 70-year-old female patient presented with a missing tooth. Her dentist assured the patient that her tooth could be replaced and presented the range of available treat- ment options. She could have a fixed bridge that would require cutting and preparing the healthy adjacent teeth, or she could replace her tooth with a Maryland-type bridge with extending wings that would be cemented to the lingual side of her adja- cent teeth. The least appealing of the options was to make a removable tooth that would be held by friction and that might ultimately require a clasp design that would keep the remov- able more firmly in place. Because of her limiting bone and the restrictive space, the author recommended the more eco- nomical procedure for replacing her tooth with a porcelain crown supported by a narrow diameter implant (Dentatus ANEW). She ultimately selected to have her tooth replaced with a porcelain crown. She was much relieved to hear that the cost would be within her means and that this would be accom- plished speedily within a fewer number of visits and in a pain- less manner.
3.
1. Considerable undercut in the anterior maxilla
2. Placement of four Atlas implants
3. Panorex of implants in place
1. 2.
3.
4.
1. The root was extracted in a straight, upward motion and the area was allowed to mature and fully heal
2. The manual winged key was used to complete the installation
3. A temporary polycarbonate crown was selected to fit into the space 4. After osseointegration, the final crown was copied from the patient’s fractured tooth
Overdentures in patients with anatomical limitations
Case courtesy of Dr. Tera Greene, Meridian, ID
A 54-year-old female presented with autoimmune hepatitis and was on heavy doses of prednisone, causing extreme dry mouth that resulted in teeth becoming grossly carious. The patient opted for full-mouth extractions and complete im- mediate dentures retained by four Dentatus Atlas implants; 2.2 x 10 mm was selected for both posterior implants and 1.8 x 10 mm for anterior implants. Dentatus implants were selected because the patient had a considerable anterior ridge undercut and the Tuf-Link silicone reline was ideal to regain her comfort.
1. 2.
Overdentures in patients with limited finances
Case courtesy of Paresh Shah, DMD, Winnipeg, Canada. Case originally appeared in Oral Health, July 2008. A 76-year-old male presented with three remaining lower anterior teeth that required extractions. The teeth were non- salvageable. He had been wearing an ill-fitting partial denture for many years. His health was noncontributory expect for one prophylactic aspirin tablet daily. His major complaint was a lower denture that was not secure enough to allow him to eat and speak properly. Several treatment options were presented including conventional implant placement (as the ideal sce- nario) or the option of a more conservative implant procedure utilizing narrow diameter implants with a minimally invasive surgical procedure. The patient selected to use narrow diameter implants due to cost, ease of placement, and the ability to function immediately.
1. Edentulous ridge prior to implant surgery
2. All four implants placed in position without raising a flap
3. The denture base was prepared and retrofitted with the resilient Tuf-Link liner
4. Patient reported denture was comfortable and secure, and that he was able to speak and eat better than prior to treatment Temporization during ridge augmentation Case courtesy of Ziv Mazor, DMD Tel Aviv, Israel
A 55-year-old woman presented with severe ridge atrophy, needing bilateral ridge augmentations and sinus lifts. Postex- traction treatment plan options were discussed with the patient during initial evaluation; a fixed implant-supported restora- tion was selected in order to achieve undisturbed healing and prevent migration of grafting material. Dentatus ANEW implants were selected as anchors for the temporary prosthe- sis due to the screw-retained feature, as the temporary bridge would need to be removed several times throughout treatment. 2.2 x 10 mm ANEW implants were inserted—two posteriorly on the right side and one anteriorly on the left, which securely held the temporary bridge
FUTURE CONSIDERATIONS
In recent years, we’ve seen an increased focus on health-care reform. In this economic climate and with the cost of health care constantly on the rise, dentists are rapidly becoming more proactive in considering alternative treatment modalities that offer solutions when patient objections limit access to care. According to Dr. Carl Misch, there is an ever-increasing demand for dental implants resulting from the combined effects of several factors, most notably that our aging population is living longer and is more socially active.32
With an increasingly aging population, higher costs of health care, and an overwhelming 90% of people rejecting implant treatment, it is time to embrace change to treat more patients with reliable, safe, and economical options.
Consider the social implications for seniors who look forward to meeting their friends for lunch or attending family celebrations—or even those at the opposite end of the spectrum—teens with congenitally missing laterals or sports injuries who are even more apt to feel self-conscious or excluded. Education is essential. Even if dentists are not placing implants themselves, they need to recognize when implants should be recommended.
For dentists looking to treat more patients, narrow diameter implants are an essential part of the implant armamentarium.
Patients report overwhelmingly of their improved quality of life and express their appreciation for treatment that they once thought was impossible.
67 MDI ClinicalStudies from AroundTheWorld
Quebec,Canada 2017
https://www.ncbi.
nlm.nih.gov/pmc/art
icles/PMC5411366/
Osseointegration of standard and mini dental implants:
a histomorphometric comparison
Jagjit S. Dhaliwal, Rubens F. Albuquerque, Jr, […], and Jocelyne S. Feine
1Faculty of Dentistry, McGill University, 2001 McGill College Avenue, Suite 500, Montreal, Quebec H3A 1G1 Canada
Abstract
Background
Mini dental implants (MDIs) are becoming increasingly popular for rehabilitation of edentulous patients because of their several advantages. However, there is a lack of evidence on the osseointegration potential of the MDIs. The objective of the study was to histomorphometrically evaluate and compare bone apposition on the surface of MDIs and standard implants in a rabbit model.
Methods
Nine New Zealand white rabbits were used for the study to meet statistical criteria for adequate power. Total 18 3M™ESPE™ MDIs and 18 standard implants (Ankylos® Friadent, Dentsply) were inserted randomly into the tibia of rabbits (four implants per rabbit); animals were sacrificed after a 6-week healing period. The specimens were retrieved en bloc and preserved in 10% formaldehyde solution. Specimens were prepared for embedding in a light cure acrylic resin (Technovit 9100). The most central sagittal histological sections (30–40 μm thick) were obtained using a Leica SP 1600 saw microtome. After staining, the Leica DM2000 microscope was used, the images were captured using Olympus DP72 camera and associated software. Bone implant contact (BIC) was measured using Infinity Analyze software.
Results
All implants were osseointegrated. Histologic measures show mineralized bone matrix in intimate contact with the implant surface in both groups. The median BIC was 58.5 % (IQR 8.0) in the MDI group and 57.0 % (IQR 5.5) in the control group (P > 0.05; Mann-Whitney test). There were NO STATISTICAL DIFFERENCES in osseointegration at 6 weeks between MDIs and standard implants in rabbit tibias.
Conclusions
Based on these results, it is concluded that osseointegration of MDIs is SIMILAR to that of STANDARD implants.
68 MDI ClinicalStudies from AroundTheWorld
Vitoria,Spain 2016
Long-Term Follow-Up of 2.5-mm Narrow-Diameter Implants Supporting a Fixed Prostheses.
Anitua E, et al. Clin Implant Dent Relat Res. 2016.
https://www.ncbi
.nlm.nih.gov/m/pubm
ed/25913652/
Authors
Anitua E1,2, Saracho J2, Begoña L2, Alkhraisat MH2.
Author information
1
Oral implantology, Eduardo Anitua Foundation, Vitoria, Spain.
2
Eduardo Anitua Foundation, Vitoria, Spain.
Citation
Clin Implant Dent Relat Res. 2016 Aug;18(4):769-77. doi: 10.1111/cid.12350. Epub 2015 Apr 27.
Abstract
BACKGROUND: The use of narrow-diameter implants (NDIs; <3.75 mm) constitutes an alternative to bone augmentation procedure. Long-term evaluation of NDIs with a diameter <3.0 mm is still lacking.
PURPOSE: Analyze the long-term outcomes of 2.5-mm NDIs splinted to regular-sized implants for supporting partial and complete fixed prostheses.
MATERIALS AND METHODS: Patients charts were retrospectively analyzed to select patients treated by the insertion of at least one 2.5-mm two-piece implant before July 2005. The study was based on the available charts (no patient was recalled). Patient’s demographic data were described. The known implant length was used as a reference to calibrate the linear measurements of marginal bone loss on digital periapical radiograph. Implant details, survival and prosthetic complications were analyzed.
RESULTS: Thirty-seven 2.5-mm implants placed in 20 patients (mean age at surgery: 54.05 ± 9.7 years) in maxilla and mandible were included and evaluated. The implants’ mean follow-up time since insertion was 6.5 ± 3.2 years (range 0 to 9.7 years). The follow-up time was more than 7 years for 22 implants. One implant failed due to lack of osseointegration. Two prosthetic complications (connector and porcelain fracture) occurred. The survival rate was 97.3% for implants and 92.0% for prostheses. The mean marginal bone loss at the mesial and distal aspect was 0.70 ± 0.55 and 0.72 ± 0.56 mm, respectively.
CONCLUSIONS: When dental implants of 2.5 mm in diameter are splinted by a fixed prosthesis, long-term favorable outcomes could be obtained.
69 MDI ClinicalStudies from AroundTheWorld
Bologna,Italy 2017
https://www.ncbi.
nlm.nih.gov/m/pub
med/25913652/
Narrow- (3.0 mm) Versus Standard-Diameter (4.0 and 4.5 mm) Implants for Splinted Partial Fixed Restoration of Posterior Mandibular and Maxillary Jaws: A 5-Year Retrospective Cohort Study.
Pieri F, et al. J Periodontol. 2017.
Authors
Pieri F1, Forlivesi C1, Caselli E2, Corinaldesi G3.
Author information
1
Private practice, Cesena, Italy.
2
Private practice, Ancona, Italy.
3
Department of Dental Sciences, University of Bologna, Bologna, Italy.
Citation
J Periodontol. 2017 Apr;88(4):338-347. doi: 10.1902/jop.2016.160510. Epub 2016 Nov 18.
Abstract
BACKGROUND: Evidence concerning predictability of narrow-diameter implants (NDIs) (<3.3 mm) to restore partially edentulous posterior maxillary and mandibular areas is limited. The aim of this study is to compare the 5-year outcomes of NDIs (3.0 mm) and standard-diameter implants (SDIs) (4.0 to 4.5 mm) supporting fixed partial dentures (FPDs) in posterior mandibular and maxillary jaws.
METHODS: All patients treated with at least two adjacent NDIs or SDIs according to available bone thickness and with a minimum follow-up of 5 years after placement were invited to undergo a clinical and radiologic examination. Outcome measures were implant and FPD failures, biologic and prosthetic complications, and marginal bone loss.
RESULTS: A total of 107 out of 127 patients attended the examination: 49 (113 implants) of the NDI group, and 58 (126 implants) of the SDI group. Two NDIs failed in one patient versus four SDIs in four patients (P = 0.37). One FPD failed in the NDI group versus two FPDs in the SDI group (P >0.99). Nine biologic complications occurred in the NDI group and twelve in the SDI group (P = 0.81). Twelve prosthetic complications occurred in the NDI group and only two in the SDI group (P = 0.001). Peri-implant marginal bone loss at 5 years was 0.95 ± 0.84 mm for the NDI group and 1.2 ± 0.86 mm for the SDI group (P = 0.06).
CONCLUSION: Five-year data indicate that FPD treatment in posterior mandibular and maxillary jaws with NDIs was as reliable as with SDIs, although NDIs showed a higher risk of prosthetic complications.
70 MDI ClinicalStudies from AroundTheWorld
Mansaura,Egypt 2011
The clinical and radiographic outcome of immediately loaded mini implants supporting a mandibular overdenture. A 3-year prospective study.
Elsyad MA, et al. J Oral Rehabil. 2011.
Authors
Elsyad MA1, Gebreel AA, Fouad MM, Elshoukouki AH.
Author information
1
Department of Removable Prosthodontics, Faculty of Dentistry, Mansoura University, Mansoura, Egypt. m_syad@mans.edu.eg
Citation
J Oral Rehabil. 2011 Nov;38(11):827-34. doi: 10.1111/j.1365-2842.2011.02213.x. Epub 2011 Mar 24.
Abstract
This article aimed to examine the clinical and radiographic outcome of mini dental implants (MDIs) supporting a mandibular overdenture. Twenty-eight patients (16 men and 12 women) complaining from insufficient retention of their mandibular denture received a total of 112 MDIs (four per patient) in the interforaminal area of the mandible using the non-submerged flapless surgical approach. Implants were immediately loaded with mandibular overdentures after implant insertion. Each implant was evaluated at the time of initial prosthetic loading, 6, 12, 24 and 36 months thereafter. Clinical evaluation was performed using plaque index (PI), gingival index (GI), probing depth (PD) and periotest values (PTVs). Radiographic evaluation was performed in terms of vertical (VBLO) and horizontal (HBLO) alveolar bone loss. Cumulative success and survival rates were calculated using life table analysis. Plaque index, GI, PD, VBLO and HBLO increased significantly in the first year after overdenture insertion, and no significant difference between subsequent observations was noted. Periotest values demonstrated no significant difference between observation times. The cumulative survival and success rates of MDIs were 96·4% and 92·9%, respectively. Within the limitations of this study, clinical and radiographic peri-implant tissue responses of immediately loaded MDIs supporting a mandibular overdenture were favourable after 3 years. However, randomised, controlled clinical trials are needed to compare these responses to that of conventional-diameter implants.
71 MDI ClinicalStudies from AroundTheWorld
Campinas Piracicaba, SP, Brazil 2018
Mini-implants and narrow diameter implants as mandibular overdenture retainers: A systematic review and meta-analysis of clinical and radiographic outcomes.
Review article
Marcello-Machado RM, et al. J Oral Rehabil. 2018.
Authors
Marcello-Machado RM1, Faot F2, Schuster AJ3, Nascimento GG4, Del Bel Cury AA5.
Author information
1
Department of Prosthodontics and Periodontology, Piracicaba Dental School, State University of Campinas Piracicaba, SP, Brazil.
2
Department of Restorative Dentistry, School of Dentistry, Federal University of Pelotas, Pelotas, RS, Brazil.
3
Graduate Program in Dentistry, School of Dentistry, Federal University of Pelotas, Pelotas, RS, Brazil.
4
Department of Dentistry and Oral Health, Aarhus University, Aarhus, Denmark.
5
Department of Prosthodontics and Periodontology, Piracicaba Dental School, State University of Campinas, Piracicaba, Brazil.
Citation
J Oral Rehabil. 2018 Feb;45(2):161-183. doi: 10.1111/joor.12585. Epub 2017 Dec 2.
Abstract
This study reviews the clinical and radiographic outcomes of Mini-implants (MI) and Narrow Diameter Implants (NDI) as mandibular overdenture (MO) retainers. Six databases were consulted for clinical studies that evaluated implants with diameter ≤3.5 mm. Data on the MI and NDI for survival and success rate and peri-implant bone loss and were collected and submitted to meta-analysis. Thirty-six studies were included, 24 reporting MI performance and 12 describing NDI results. The MI group comprised data from 1 cross-sectional clinical study, 3 retrospective longitudinal (RL) clinical studies, 13 prospective longitudinal (PL) clinical studies and 7 randomised clinical trials (RCT) with follow-up periods ranging from 1 day to 7 years. Eight studies used conventional loading, thirteen used immediate loading, two studies used both loading types, and one study did not report. The NDI group comprised data from 3 RL clinical studies, 6 PL clinical studies and 3 RCT with follow-up ranging from 6 months to 10 years. Ten studies used conventional loading, 1 study used immediate loading, and 1 study did not report. The average survival rates of MI and NDI studies were 98% and 98%, respectively, while the average success rates were 93% and 96%, respectively. The average peri-implant bone loss after 12, 24 and 36 months was 0.89, 1.18 and 1.02 mm for MI and 0.18, 0.12 and -0.32 mm for NDI. Both MI and NDI showed adequate clinical behaviour as overdenture retainers. The NDI showed a better long-term predictability to retain OM with most studies adopting conventional loading. PMID 29125652 [Indexed for MEDLINE]
72 MDI ClinicalStudies from AroundTheUSA
New York,NY 2007
Narrow-diameter implants: a restorative option for limited interdental space.
Froum SJ, et al. Int J Periodontics Restorative Dent. 2007.
Authors
Froum SJ1, Cho SC, Cho YS, Elian N, Tarnow D.
Author information
1
Department of Periodontology and Implant Dentistry, College of Dentistry, New York University, New York, NY, USA. dr.froum@verizon.net
Citation
Int J Periodontics Restorative Dent. 2007 Oct;27(5):449-55.
Abstract
The present study reports on the results of the use of a screw-retained narrow-diameter implant (NDI) system as an option for implant placement in areas of limited bone volume. This retrospective report followed 48 NDIs in 27 patients for 1 to 5 years postloading. No implant failures were reported, yielding a 100% survival rate. The screw-retained attribute of this system allows retrievability of the restorations, which may require replacement because of porcelain fracture, chipping, or a desire to change color. The three diameters available–1.8 mm, 2.2 mm, and 2.4 mm–allow flexibility for a variety of narrow edentulous spaces. These NDIs present a cost-effective alternative for restoring limited spaces with implant restorations, without the bone augmentation or orthodontic procedures required for conventional fixed restorations. The NDI system is approved by the U.S. Food and Drug Administration for long-term use.
73 MDI ClinicalStudies from AroundTheWorld I
Istanbul, Turkey 2007
Treatment of a narrow, single tooth edentulous area with mini-dental implants: a clinical report.
Dilek OC, et al. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007.
https://www.ncbi
.nlm.nih.gov/m/pub
med/17095267/?i=
2&from=/16704110
/related
Authors
Dilek OC1, Tezulas E.
Author information
1
Oral Implantology, Faculty of Dentistry, Yeditepe University, Istanbul, Turkey. ozkand@yeditepe.edu.tr
Citation
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Feb;103(2):e22-5. Epub 2006 Nov 7.
Abstract
The narrowing of an extraction site often becomes problematic when attempting to restore the space with a conventional wide-diameter implant. A woman is presented who was treated with a square head, mini-dental implant-supported fixed denture for a maxillary with a narrowed edentulous area, with a mesiodistal width of 5 mm. The implant, with a diameter of 2.4 mm, was inserted without reflecting the mucoperiosteal flap and was loaded immediately. During 12 months of follow-up, there has been no bone resorption and no inflammation observed around the implant. In conclusion, in terms of both clinical and aesthetic criteria, small diameter, mini-dental implants can be successfully used as an alternative to treatment with fixed partial dentures. PMID 17095267 [Indexed for MEDLINE]
74 MDI ClinicalStudies from AroundTheWorld
Seoul,Korea 2012
Long‐term retrospective study of narrow implants for fixed dental prostheses
Jung‐Seok Lee Hyun‐Min Kim Chang‐Sung Kim Seong‐Ho Choi Jung‐Kiu Chai Ui‐Won Jung April 2012
https://doi.org/10
.1111/j.1600-0501
.2012.02472.x
Abstract
Objective
The objectives of this study were to analyze retrospectively the long‐term survival and success rates of Narrow implants (NIs) placed with various implant systems, and the association with biological and technical complications.
Material and methods
In total, 338 patients (men = 45.6%, women = 54.4%) who received 541 NIs (≤3.5 mm in diameter) for fixed prostheses were enrolled in this retrospective study. The mean marginal bone level (MMBL) change was calculated. Life table analysis with the cumulative survival rate and success rate was calculated, and biological and technical complications were evaluated.
Results
The annual MMBL change was 0.07 ± 0.20 mm. The 12‐year cumulative survival (success) rates of NIs were 98.1% (91.8%) and 98.5% (93.8%) for the implant‐ and subject‐based analysis, respectively. During the observation period up to 12 years (mean 4.9 years), six implants were lost in the maxilla, whereas three implants were lost in the mandible. Technical complications were more frequent than biological complications. Infection was the most common underlying cause of biological complications and the most frequent technical complication was decementation.
Conclusion
In conclusion, the findings of this study suggest that NIs could be used safely for narrow alveolar ridges or narrow mesiodistal spaces on the basis of their high survival rate.
75 MDI ClinicalStudies from AroundTheUSA
New York,NY 2007
Immediate loading of narrow-diameter implants wit in severely atrophic mandibles.
Cho SC, et al. Pract Proced Aesthet Dent. 2007.
Authors
Cho SC1, Froum S, Tai CH, Cho YS, Elian N, Tarnow DP.
Author information
1
Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, NY, USA. Citation
Pract Proced Aesthet Dent. 2007 Apr;19(3):167-74.
Abstract
Oral rehabilitation using two to four implants to support mandibular overdentures has been shown to have success rates of approximately 96% with implants placed in a one- or two-stage procedure. The purpose of this study is to evaluate 10 consecutive cases of immediately loaded, narrow-diameter implants (NDIs) as support for overdentures in severely atrophic mandibles, and report on implant/prosthetic survival rates and patient satisfaction. Overall implant and prosthetic survival rates were 94.1% and 100%, respectively. PMID 17511121 [Indexed for MEDLINE]
76 MDI ClinicalStudies from AroundTheWorld
Boston,Mass
São Paulo,Brazil 2017
Narrow‐ and regular‐diameter implants in the posterior region of the jaws to support single crowns: A 3‐year split‐mouth randomized clinical trial
André Barbisan de Souza Flávia Sukekava Livia Tolentino …
https://onlinelibrary
.wiley.com/doi/abs/
10.1111/clr.13076#
Abstract
Objectives
The objective of this 3‐year split‐mouth randomized controlled clinical study was to compare narrow‐diameter implants (NDIs) to regular‐diameter implants (RDIs) in the posterior region of the jaws (premolars and molars) in regards to (i) the marginal bone level (MBL) and (ii) implant and prosthesis survival and success rates.
Material and Methods
A total of 22 patients were included in the study. Each patient received at least one implant of each diameter (Ø3.3 and Ø4.1 mm), placed either in the maxilla or mandible to support single crowns. A total 44 implants (22 NDIs and 22 RDIs) were placed and included in the study. Twenty‐one implants were placed in the premolar, whereas 23 were placed in molar areas. Radiographic evaluations to access the MBL were performed immediately after implant placement, 1 and 3 years after implant loading. Peri‐implant clinical variables including probing pocket depth (PPD) and bleeding on probing (BoP) were obtained after crown delivery, 1 and 3 years after loading. Furthermore, the survival and success rates of the implants and prosthesis were also evaluated.
Results
Twenty patients were able to complete the study. There was no statistically significant difference regarding MBL between groups at implant placement (p = .084), 1‐year (p = .794) and 3‐year (p = .598) time intervals. The mean peri‐implant bone loss at 3‐year follow‐up was −0.58 ± 0.39 mm (95% CI: −0.751 to −0.409) and −0.53 ± 0.46 mm (95% CI: −0.731 to −0.329) for NDIs and RDIs, respectively. BoP was present at 15% and 10% of NDIs and RDIs, respectively, at 3‐year follow‐up. PPD >5 mm was observed in 5% and 0% of the implants of NDIs and RDIs, respectively, at 3‐year follow‐up. At the 3‐year examination, the implant success rates were in the NDIs and RDIs sites, respectively, 95% and 100%. The corresponding values for prosthesis success rates were 90% for NDIs and 95% for RDIs.
Conclusion
The present study demonstrated that NDIs placed to support single crowns in the posterior region … DID NOT DIFFER to RDIs in regards to MBL, implant survival, and success rates.
77 MDI ClinicalStudies from AroundTheUSA
New York,NY 2007
Long-Term Retrospective Evaluation of Success of Narrow-Diameter Implants in Esthetic Areas: A Consecutive Case Series with 3 to 14 Years Follow-up.
Froum SJ, et al. Int J Periodontics Restorative Dent. 2017 Sep/Oct.
Show full citation
https://www.ncbi.nlm.nih.gov/m/pubmed/28817125/
Abstract
This retrospective study reports on the outcome of 19 narrow-diameter implants (NDIs) placed in 14 consecutively treated patients 3 to 14 years postloading. Peri-implant bone remodeling, bone loss, esthetic outcomes, and patient satisfaction with the final restoration were evaluated. No implant failures or prosthetic complications were reported, yielding a 100% survival rate and a 84.2% success rate. All 14 patients reported that they were very satisfied with the esthetic results. The average mesial and distal bone remodeling was 1.99 mm and 1.84 mm, respectively. This represents physiologic bone loss post-implant placement. Only 5 implants presented with bone loss, producing an average mesial and distal bone loss of 0.14 mm and 0.17 mm, respectively. Bone loss was measured on the threads of the implant from the time of restoration to the time of follow-up. The bone loss did not exceed 0.2 mm per year on any implant. These screw-retained NDIs present a cost-effective, esthetically acceptable alternative for restoring limited spaces in the anterior esthetic zone.
78 MDI ClinicalStudies from AroundTheUSA
New York,NY 2007
Narrow-diameter implants: a restorative option for limited interdental space.
Froum SJ, et al. Int J Periodontics Restorative Dent. 2007.
Abstract
The present study reports on the results of the use of a screw-retained narrow-diameter implant (NDI) system as an option for implant placement in areas of limited bone volume. This retrospective report followed 48 NDIs in 27 patients for 1 to 5 years postloading. No implant failures were reported, yielding a 100% survival rate. The screw-retained attribute of this system allows retrievability of the restorations, which may require replacement because of porcelain fracture, chipping, or a desire to change color. The three diameters available–1.8 mm, 2.2 mm, and 2.4 mm–allow flexibility for a variety of narrow edentulous spaces. These NDIs present a cost-effective alternative for restoring limited spaces with implant restorations, without the bone augmentation or orthodontic procedures required for conventional fixed restorations. The NDI system is approved by the U.S. Food and Drug Administration for long-term use.
79 MDI ClinicalStudies from AroundTheWorld
Bologna,Italy2009
Immediate restoration of small-diameter implants in cases of partial posterior edentulism: a 4-year case series.
Degidi M, et al. J Periodontol. 2009.
https://www.ncbi
.nlm.nih.gov/pub
med/19485833/
Authors
Degidi M1, Nardi D, Piattelli A.
Author information
1
Private practice, Bologna, Italy.
Citation
J Periodontol. 2009 Jun;80(6):1006-12. doi: 10.1902/jop.2009.080649.
Abstract
BACKGROUND: The aim of this prospective study was to evaluate the use of immediate restorations supported by 3.0-mm-diameter implants as a suitable technique for the rehabilitation of partial posterior edentulism.
METHODS: Forty consecutive patients, 18 males and 22 females with a mean age of 54.7 +/- 17.2 years, with partial edentulism in the posterior region were treated with 93 immediately restored 3.0-mm-diameter implants. Forty-eight and 45 implants were placed in the maxilla and mandible, respectively. All implants were placed in healed sites and splinted by the temporary restoration, which was placed to avoid occlusal contact. The final restoration was delivered approximately 6 months after implant insertion. Mean marginal bone loss was assessed using standard periapical radiographs immediately after surgery and at 6-, 12-, 24-, 36-, and 48-month follow-up examinations.
RESULTS: All implants had osseointegrated and were clinically stable at the 6-month follow-up. The accumulated mean marginal bone loss was 1.16 +/- 0.90 mm (N = 89) at the 48-month follow-up. No implant fractures occurred.
CONCLUSION:
The use of immediately loaded small-diameter implants supporting fixed partial restorations is a predictable procedure for the rehabilitation of partial posterior edentulism.
80 MDI ClinicalStudies from AroundTheWorld
Milan ,Italy2009
Clinical and Radiographic Evaluation of a Small-Diameter Dental Implant Used for the Restoration of Patients with Permanent Tooth Agenesis (Hypodontia) in the Maxillary Lateral Incisor and Mandibular Incisor Regions: A 36-Month Follow-Up.
King P, et al. Int J Prosthodont. 2016 Mar-Apr.
https://www.ncbi.nlm.nih.gov/pubmed/26929953/
Authors
King P, Maiorana C, Luthardt RG, Sondell K, Øland J, Galindo-Moreno P, Nilsson P.
Citation
Int J Prosthodont. 2016 Mar-Apr;29(2):147-53. doi: 10.11607/ijp.4444.
Abstract
PURPOSE: For patients with narrow, single-tooth edentulous ridges as a result of permanent tooth agenesis (hypodontia) in the maxillary lateral and mandibular incisor regions, dental implant treatment may present a reliable and predictable restorative treatment solution. The aim of the present study was to evaluate the clinical reliability and outcome of small-diameter dental implants placed in a one-stage procedure with early loading replacing maxillary lateral or mandibular incisor teeth.
MATERIALS AND METHODS: Patients with hypodontia in the maxillary lateral incisor or mandibular incisor region analyzed in this report were selected from a larger prospective multicenter study. Small-diameter dental implants (AstraTech OsseoSpeed TX 3.0 S, Dentsply) of different lengths were placed using a one-stage surgical protocol with a 6- to 10-week healing period before loading. Probing pocket depth, bleeding on probing, and gingival zenith score were assessed after 6, 12, 24, and 36 months. Radiographic examination was assessed at 6, 12, and 36 months.
RESULTS: In total, 38 patients were included in this analysis and 62 small-diameter implants were placed. The mean distance between adjacent teeth was 6.30 mm (SD: 1.36). All patients received a titanium transmucosal abutment and cement-retained ceramic crown after 6 to 10 weeks of healing. Two implants were lost during the healing period before loading, providing a total implant survival rate of 96.8%. No implant fractures were reported. Mean marginal bone level change from surgery to follow-up visits at 6, 12, and 36 months were 0.39 mm, 0.22 mm, and 0.23 mm, respectively. The condition of soft tissue was stable at all follow-up visits with clinically insignificant changes in probing depth, bleeding on probing, and gingival zenith score.
CONCLUSION: This study evaluated the behavior over 36 months of AstraTech Osseospeed TX 3.0 S dental implants placed into narrow one-tooth defect edentulous ridges as a result of hypodontia. The data collected highlighted the stability of the marginal bone level and soft tissues around the dental implants in conjunction with durable mechanical function. Small-diameter implants can be considered a valid solution in the restorative treatment of hypodontia in the maxillary lateral and mandibular incisor regions. PMID 26929953 [Indexed
81 MDI ClinicalStudies from AroundTheWorld
Padova ,Italy 2004
Clinical evaluation of small-diameter implants in single-tooth and multiple-implant restorations: a 7-year retrospective study.
Vigolo P, et al. Int J Oral Maxillofac Implants. 2004 Sep-Oct.
https://www.ncbi
.nlm.nih.gov/pub
med/15508986/
Abstract
PURPOSE: Placement of small-diameter implants often provides a solution to space-related problems in implant restoration. This 7-year retrospective study presents results from 192 small-diameter implants placed in 165 patients from 1992 to 1996.
MATERIALS AND METHODS: The dental records of each patient were reviewed. The implants, which were either 2.9 mm or 3.25 mm in diameter, were placed by 2 different surgeons. All prosthetic appliances were fabricated by the same prosthodontist. Ninety-four implants supported single-tooth cemented restorations; the remaining 98 implants supported cemented or screw-retained partial prostheses.
RESULTS: The total implant survival rate was 95.3%. Four implants were lost at second-stage surgery, and 5 more were lost after loading.
DISCUSSION: Small-diameter implants demonstrated a survival rate similar to those reported in previous studies of standard-size implants.
CONCLUSIONS: The results suggest that small-diameter implants can be successfully included in implant treatment. They may be preferable in cases where space is limited.
82 MDI ClinicalStudies from AroundTheWorld
Vincenza,Italy 2000
Clinical evaluation of single-tooth mini-implant restorations: a five-year retrospective study.
Vigolo P, et al. J Prosthet Dent. 2000.
https://www.ncbi.nlm.nih.gov/pubmed/10898842/
Abstract
STATEMENT OF PROBLEM: Placement of small diameter implants often provides a solution to space problems in implant restoration. Analysis of the success of this type of implant restoration has not been clearly determined. PURPOSE: This 5-year retrospective study presents results from 52 mini-implants for single-tooth restorations placed in 44 patients from 1992 to 1994. MATERIAL AND METHODS: Dental records of 44 patients with 52 mini-implants placed during 1992-94 were reviewed. The implants were all placed by the same surgeon and the single-tooth custom screwed posts with cemented crowns were positioned on the implants by the same prosthodontist. RESULTS: The results achieved by the mini-implant rehabilitation were similar to those reported for standard single-tooth implant restoration. Total implant survival rate was 94.2%. Two implants were lost at second stage surgery, and another was lost after temporary loading. CONCLUSION: The results suggest that single-tooth mini-implant restoration can be a successful treatment alternative to solve both functional and esthetic problems. They may represent the preferred choice in cases where space problems limit the use of standard or wide diameter implants. PMID 10898842 [PubMed – indexed for MEDLINE]
83 MDI ClinicalStudies from AroundTheUSA
Newport Beach,Ca 2015
Bicortical Stabilization
Dr Paresh Patel – GlidewellLab
Small Diameter Implants: Choosing the Appropriate Implant Diameter
Inclusive Magazine: Volume 4, Issue 1
Bicortical Stabilization
Engaging the bone in both directions (labio-lingual) as well as the inferior and superior plates is important when choosing the appropriate implant diameter. That is where mini implants are at their best: placed in thin bone with strong cortical plates — the ideal environment for a small-diameter implant to engage and osseointegrate.
Availability of Bone
Conventional diameter implants… typically require at least 6 mm of width labio-lingually. But most patients who need denture stabilization LACK SUFFICIENT BONE WIDTH for these larger root-form fixtures, necessitating either a ridge augmentation procedure or the placement of SMALL-diameter implants.
Mini implants… can often be placed in as little as 3 mm of bone, gaining stability by engaging both labial and lingual cortical plates. Similarly, a mini implant of just 10 mm in length can be sufficient to achieve bicortical stabilization along the inferior-superior axis in a resorbed mandible.
Bicortical Stabilization of Inclusive® Mini Implants in the Labio-Lingual Dimension
Quality of Bone
Generally accepted PLACEMENT PROTOCOLS suggest that the widest possible diameter of implant be used based on the available bone. However, the TREAD DESIGN of various implant sizes may also be taken into account in relation to the quality of bone. A THINNER RIDGE often indicates a higher percentage of CORTICAL BONE and associated bone density. A THICKER RIDGE often indicates a higher percentage of CANCELLOUS interior bone. The increasing thread pitch associated with successively wider Inclusive® Mini Implants reflects an anticipation of the bone density to be encountered with various ridge sizes. Naturally, it is incumbent upon the clinician to treatment plan for the ideal implant size on a case-by-case basis, based on a complete diagnostic evaluation. The variation in thread design referenced above is chiefly intended to facilitate efficient placement in various bone types as commonly encountered.
The INCREASING THREAD PITCH associated with successively wider Inclusive Mini Implants reflects an anticipation of the BONE DENSITY to be encountered with VARIOUS RIDGE SIZES .
Naturally, it is incumbent upon the clinician to treatment plan for the ideal implant size on a case-by-case basis, based on a complete diagnostic evaluation. The variation in thread design referenced above is chiefly intended to facilitate efficient placement in various bone RIDGE SIZES . Note: The 3.0 Inclusive Mini Implant is used to compress, condense and engage Type D2 bone. Because it is a SELF-TAPPING SCREW, removing the entire volume of bone, as in the case of a TRADITIONAL implant with a NON-CUTTING APEX…is NOT NECESSARY.
Ø 2.2 mm Inclusive Mini Implant for Types D1 and D2 Bone, Respectively
Other Factors for Consideration
1)NUMBER of IMPLANTS–
As important as the diameter, the standard number of mini implants is typically FOUR (4) in the LOWER arch and SIX (6) in the UPPER arch.
2)GREATER STABILITY-
If possible, placing FIVE (5) in the LOWER and SEVEN (7) in the UPPER and engaging additional alveolar bone will lend GREATER STABILITY.
3)IMMEDIATE LOADING –
If 35 Ncm of torque can be achieved, it is generally safe to load the mini implants with a new denture featuring O-ring attachment housings, or to pick up the housings in an existing denture chairside. If achieving 35 Ncm of torque is not possible, consider a soft reline of the denture and allow for a prescribed period of osseointegration.
4)PARAFUCTIONAL HABITS –
Lateral forces can compromise the success of any implant, so if the patient is a BRUXER or GRINDER, consider placing the LARGEST diameter implant possible.
5)OCCLUSION–
Whether mini implants are being placed in the upper or the lower arch, if the opposing arch is natural dentition and 35 Ncm of torque cannot be achieved for all implants, consider soft lining the denture for six weeks.
6)A-P spread –
The wider the anterior-posterior (A-P) spread, the more stable the oral environment.
o Upper arch: Maximize the A-P spread by placing the most distal implants as far back as possible without impinging on the sinus cavities
o Lower arch: Try to space posterior implants 5 mm anterior to the mental foramen.
Serving a Changing Demographic
As a population, we are simply living longer, and the number of older people will increase dramatically over the next few decades. Statistics say 10,000 Americans are turning 65 daily, with 40 million people estimated to be edentulous.* Clearly, it’s TIME for us to fully embrace the idea of mini implants as a viable treatment option for these older patients.
BONE RESORPTION …
is more commonplace among aging patients, and small-diameter implant placement protocols represent a MINIMALLY INVASIVE , MORE AFFORDABLE …ALTERNATIVE to conventional-diameter implant placement.
Ø 2.5 mm Inclusive Mini Implant for Highly Resorbed Premaxilla Bone
84 MDI ClinicalStudies from AroundTheUSA
Newport Beach,Ca 2016
Achieving Success with Small-Diameter Implants
Chairside Magazine: Volume 10, Issue 1
article by Paresh B. Patel, DDS
It is without question that dental implants are one of the most successful additions to modern dentistry. With a success rate of greater than 95 percent, the root-form implant should be considered to restore any edentulous area. However, when we are presented with the need to manage a highly resorbed ridge, significant issues for the surgeon and restorative team arise if only the use of a standard body implant (3.7 mm or larger) is considered. These issues can be anatomical, medical, financial or restorative. Anatomical challenges are closely associated with how much residual alveolar ridge remains (quantity) and also its density (quality). These can sometimes be overcome with additional surgical procedures such as ridge expansion, block grafting, and other hard- and soft-tissue procedures. If these solutions are not accepted, the use of a much less invasive procedure should be considered, such as the small-diameter implant (SDI), also referred to as the mini implant. SDIs have been around in their FDA-approved form since 1997 and share surface texture, coatings and titanium grade similar to their larger counterparts. Most implant manufacturers now have added SDIs to their systems. These SDIs now are available in one- and two-piece versions as well as crown & bridge prosthetic options. Medical challenges should be addressed by utilizing the most minimally invasive surgical plan. The incorporation of 3-D cone-beam computed tomography is rapidly increasing and can allow for presurgical planning to avoid mandatory grafting. A CBCT surgical guide can be created to deliver the implant into the bone with a flapless technique reducing surgical trauma. This may be a prudent solution for patients with systemic conditions who are unable to tolerate lengthy healing times. It is important to note that a CBCT-based surgical guide is much different from a prosthetic guide that is based on a panoramic X-ray and a stone model. A CBCT surgical guide can be created to deliver the implant into the bone with a flapless technique reducing surgical trauma. This may be a prudent solution for patients with systemic conditions who are unable to tolerate lengthy healing times. Restorative challenges are usually the management of restricted restorative space in the mesial-distal or buccal-lingual direction. This has always posed a high-risk problem in the esthetic area. Too wide of an implant will create potential for bone and soft-tissue loss. Convergent roots can also preclude the use of a standard body implant. In these cases, an SDI may allow for the placement of the implant and still allow proper bone support, soft-tissue space and proper spacing from adjacent tooth roots. SDIs can be used to retain maxillary or mandibular dentures. Due to reduced surface area, it is recommended to utilize four SDIs in the mandible and six SDIs in the maxilla. The residual ridge should be of Misch Type I or II to ensure a successful case. If the SDI selected is of a one-piece design, then immediate loading must be addressed. Primary stability should be at a minimum of 30 Ncm on all of the implants, and a stable tissue-supported denture should be delivered. The implants should also be placed as parallel as possible to minimize off-axis loads.
Case Reports
Case 1:
Multiple-Unit Fixed Restorations
Diagnosis and Treatment Planning — A 54-year-old female presented in general good health with a history of diabetes. She had progressively lost her teeth during the previous 15 years, with the last of them being extracted about five years earlier. She was unhappy with her existing dentures due to poor retention and difficulty with eating. Both ridges were examined and found to be moderately atrophic (Figs. 1, 2). A CBCT scan was taken (i-CAT® FLX [Imaging Sciences International, LLC; Hatfield, Pa.]) with the dual-scan protocol to facilitate a prosthetically driven treatment plan .
Due to the height and width of the remaining bone, six SDIs would be placed in the maxilla and four SDIs in the mandible to support overdentures. The SDIs selected for this case were of a two-piece design with a Locator® attachment (Zest Anchors LLC; Escondido, Calif.). The low profile of the attachment would allow for a less obtrusive denture and a variety of retentive inserts. After the treatment plan was approved by the patient, surgical guides (Anatomage; San Jose, Calif.) were ordered .
Clinical Protocol — On the day of surgery, the surgical guides were tried in to verify stability and fit (Figs. 7, 8). A single 1.6 mm pilot bit was used to create the osteotomies through the surgical guide in the maxilla using an implant motor (Aseptico AEU-7000 [Aseptico, Inc.; Woodinville, Wash.]) with copious irrigation (Fig. 9). The pilot guide was removed, and the implants were inserted and carried to depth (Fig. 10).
All six SDIs were confirmed to have at least 30 Ncm of torque, and the Locator attachments were secured (Fig. 11). This protocol was duplicated on the lower arch (Fig. 12). To ensure that the existing dentures would fit passively over the SDIs, Fit Test (VOCO America, Inc.; Indian Land, S.C.) material was placed and allowed to set, showing where relief areas would need to be created (Figs. 13, 14). Once the relief was complete, the process was repeated until a verified passive denture could be obtained (Figs. 15, 16). The dentures could then be soft-relined (Ufi Gel SC [VOCO America]). A final CBCT scan was taken to ensure that all of the SDIs were fully encased in bone and no vital anatomical structures were violated (Fig. 17).
All six SDIs were confirmed to have at least 30 Ncm of torque, and the Locator attachments were secured.
Case 2:
Single-Unit Fixed Prosthetics
SDIs can be an excellent solution to support a single crown in areas of reduced interdental space (less than 5 mm between adjacent teeth) where it would be impossible to place a larger implant. These areas could be maxillary lateral and mandibular incisors. Case selection should have a bone type of Misch I or II, and off-axis occlusal forces should be minimized by designing the single-unit crown to have implant-protected occlusion. The use of a single SDI to support a crown much larger than a maxillary lateral is still quite controversial. SDIs can be an excellent solution to support a single crown in areas of reduced interdental space (less than 5 mm between adjacent teeth) where it would be impossible to place a larger implant. Diagnosis and Treatment Planning — An 18-year-old presented to our office after completion of orthodontics several months prior. He had lost his retainer/flipper that also replaced his missing upper lateral #7 (Fig. 18). A digital radiograph (DEXIS Platinum Sensor [DEXIS, LLC; Hatfield, Pa.]) was taken to see the position of adjacent roots, and it confirmed an extremely narrow mesiodistal space (Fig. 19). It was decided to utilize a one-piece, 3.0-mm-diameter crown and bridge SDI (I-Mini™ One-Piece Implant System [OCO Biomedical Inc.; Albuquerque, N.M.]). The decision to use this brand was due to the I-Mini’s aggressive thread design that allows for compression and fixation of the implant in Type II bone.
Clinical Protocol —
A 1.8 mm pilot bit in the Aseptico handpiece was used to carefully create the initial osteotomy (Fig. 20) and another digital radiograph was taken to confirm a parallel path between the adjacent roots (Fig. 21). A final 2.4 mm osseoformer was used to prepare the bone, and the one-piece SDI was inserted (Fig. 22). After final depth was reached, the prosthetic head of the implant was shaped for interarch space with a high-speed handpiece (KaVo Dental; Charlotte, N.C.) and a titanium abutment prep bur (Komet USA LLC; Rock Hill, S.C.) (Fig. 23). A conventional vinyl polysiloxane (VPS) impression (Take 1™ Advanced [Kerr Corporation; Orange, Calif.]) was taken using light- and heavy-body materials. The case was then sent to our dental laboratory team for the fabrication of a monolithic zirconia crown (BruxZir® Solid Zirconia) (Fig. 24).
Case 3:
Multiple-Unit Fixed Restorations
Many of the same principles of utilizing an SDI for single-unit fixed restorations should be embodied when applying their use for multiple-unit fixed restorations. All fixed units should be splinted together to help dissipate force and minimize any micro-movement. In function, the occlusal loads can be distributed over the multiple splinted SDIs. This reduces the functional load on any one SDI and increases the bone-to-implant contact. For full-arch cases, it is prudent to increase the number of SDIs in order to reach the desired surface area to prevent implant overload.
Diagnosis and Treatment Planning — A 62-year-old female presented with the chief complaint of difficulty chewing and keeping her dentures in place. The patient stated she had been wearing the full upper and lower dentures for 15 years. The clinical exam revealed the edentulous tissue to have a healthy appearance (Fig. 25). The patient stated that her experience with dentures had made her unhappy and self-conscious with her overall appearance, so much so that she wanted to have “fixed teeth.” A medical history review revealed the patient had had a previous heart attack and continued the use of Plavix® (Sanofi US; Bridgewater, N.J.), an anticoagulant medication. The patient also had diabetes controlled with medication.
Figure 25: Pre-op maxillary ridge.
To minimize surgical trauma and to increase the efficiency of implant-guided surgery, a flapless technique was to be employed for implant placement. A CBCT scan was taken for treatment planning and fabrication of a surgical guide. Upon completion of the CT scan, it was evident that the residual ridges were highly resorbed and would require the use of SDIs or additional surgical procedures to accommodate standard body implants. To keep within our concept of minimally invasive dentistry, multiple SDIs were prescribed to support the full-arch restorations. The treatment plan options were discussed with the patient and the final decision was made and approved by the patient. CBCT surgical guides (Materialise NV; Plymouth, Mich.) were made for upper and lower full-arch implant placement.
Clinical Protocol — The patient presented on her appointed day with no changes made to her daily medication regimen. Infiltration with local anesthetic was administered. The surgical guides were tried in to ensure proper fit and stability (Figs. 26, 27). The surgical guides were retained, and a 1.8 mm pilot drill was used in each site to full length. The guides were then removed, and an immediate photograph was taken to illustrate the minimal amount of trauma to the implant surgical sites (Fig. 28). Each SDI (3.25 mm ERI [OCO Biomedical Inc.]) was started by hand to half depth (Fig. 29), and then taken to full depth using the Aseptico surgical motor. With the exception of the posterior upper right site, all sites accepted a two-piece 3.25 x 12 mm in the maxilla and 3.25 x 10 mm in the mandible (Fig. 30). A post-implant placement CT scan was taken; it demonstrated parallel placement in the panoramic view very closely resembling what was treatment planned (Fig. 31). In addition, the 3-D slice view showed that the implants were fully encased in bone, away from the nerve canal and engaging the cortical plate for maximum stability (Fig. 32). Solid abutments (OCO Biomedical Inc.) were placed and torqued to 30 Ncm. Full-arch impressions of the duplicated dentures were taken with Take 1 Advanced. The impressions were then delivered to the lab team, and full-arch fixed bridges were fabricated for final cementation .
Closing Comments
With the use of guided surgery and SDIs, more patients can undergo implant surgery to achieve their desired goals to have teeth. SDIs, along with minimally invasive dentistry, are an ideal treatment solution to consider when standard-body implants are not feasible without additional procedures. Dr. Patel is a graduate of University of North Carolina at Chapel Hill School of Dentistry and the Medical College of Georgia/American Academy of Implant Dentistry Maxi Course. He is the cofounder of the American Academy of Small Diameter Implants and is a clinical instructor at the Reconstructive Dentistry Institute. He has placed more than 2,500 mini implants and has worked as a lecturer and clinical consultant on mini implants for various companies. He can be reached at pareshpateldds2@gmail.com or dentalminiimplant.com.
85 MDI ClinicalStudies from AroundTheUSA
Utica,NY 2016
Small-Diameter Implant Treatment PlanRevision:
Management of Complications Brian J. Jackson, DDS*
http://brianjacksondds.com/wp-content/uploads/2016/07/orim-42-03-294-298-e.pdf
Small-Diameter Implant Treatment PlanRevision:
Management of Complications Brian J. Jackson, DDS*
Implant dentistry has become a predictable discipline for reconstructing the edentulous patient. The edentulous population in the United States will increase over the next 3 decades, and the demand for implant-supported prostheses will rise accordingly.1 Maxillary and mandibular implant- retained overdentures may serve as an acceptable treatment option for the rehabilitation of the edentulous patient.2,3 Conventional implants are the primary type and diameter size used in reconstruction, however small-diameter implants (SDI) or mini-dental implants (MDI) may play a role in specific indications. Survival rates for small-diameter endosseous implants demonstrate a mean success rate of 94%, although complications and failures have been reported.4,5 Reasons for less than ideal outcomes are poor diagnosis and treatment planning, inadequate bone quality/quantity, implant design, early/late loading, prosthetic design, and biomechanical factors related to implant occlusal concepts.6 This case letter describes a mini-implant failure and the subsequent management of complications and oral recon- struction for the edentulous patient with removable over- dentures. Small-diameter implants have received Food and Drug Administration approval for long term use for overdentures, removable partial dentures, and fixed multiunit bridges.7 Small- diameter implants are a 1-piece, single-stage implant manu- factured from titanium alloy. They are composed of an intraosseous, transgingival, and o-ball prosthetic component. It is essential that strict surgical and prosthetic protocols are followed or less than ideal outcomes can be realized.9
CONCLUSION
For this case report, small-diameter (,3 mm) implant failure was probably due to poor surgical placement, immediate loading, and poor occlusal design. Small-diameter implants have emerged as a possible solution for patients with deficient bone, compromised health histories, and financial limitations. The conservative body of research regarding SDI has empha- sized the importance of strict protocols to ensure predictable outcomes. Complications leading to failures or other less than ideal outcomes can lead to undesirable clinical results. A thought-provoking treatment plan revision can salvage cases and meet patient expectations.
86 MDI ClinicalStudies from AroundTheWorld
Modena, Italy 2017
Narrow implants (2.75 and 3.25 mm diameter) supporting a fixed splinted prostheses in posterior regions of mandible: one-year results from a prospective cohort study
Tommaso Grandi, Luigi Svezia, and Giovanni Grandi
International Journal of Implant Dentistry, 3, 1, (2017)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5591178/
Abstract
Background
Can multiple splinted narrow-diameter implants be used as definitive implants in patients with insufficient bone ridge thickness in posterior regions of the mandible? With this aim, we evaluated their outcomes in this set up to 1 year after loading.
Methods
Forty-two patients with a mean age of 61.3 years old (range 49–73) in need of fixed prosthetic implant-supported rehabilitations in the posterior region of the mandible, presenting a thin alveolar crest, were selected. One hundred twenty-four narrow-diameter implants (2.75 and 3.25 mm diameter) were placed and splinted with a bridge. One implant for each missing tooth was requested to be inserted. Outcomes measured were implant survival, complications, and marginal bone level changes up to 1 year after loading.
Results
At the 12-month follow-up, three implants failed. Two 2.75 mm diameter implants and one 3.2 mm diameter implant failed. The implant survival rate was 97.6%. Peri-implant bone resorption was 0.20 mm (CI 95% 0.14: 0.26) after 6 months and 0.47 mm (CI 95% 0.29; 0.65) after 12 months of loading, not different between 2.75 and 3.25 mm diameter groups (p = 0.786). Of the 42 cases, three had an episode of peri-implant mucositis (7.1%).
Conclusions
Within the limits of this study, preliminary short-term data (1 year post-loading) suggested that narrow-diameter implants (2.75 to 3.25 mm) can be successfully used as a minimally invasive alternative to horizontal bone augmentation in the posterior mandible. However, larger and longer follow-ups of 5 years or more are needed.
Keywords: Bone atrophy, Bone resorption, Dental implants, Implant failure, Narrow-diameter implants, Posterior mandible
87 MDI ClinicalStudies from AroundTheUSA
Woodstock,NY 2016
Small-Diameter Implants
01 May 2016
Michael Tischler, DDS
DentistryToday
Much has changed during the past 10 years with respect to SDIs. Years ago, they would have only referred to mini one-piece implants to support an overdenture. Now SDIs include one- and 2-piece implants, offering choices for both removable and fixed prosthetic options. This month’s Implants Today topic is “Small-Diameter Implants,” or SDIs. Much has changed during the past 10 years with respect to this topic. Years ago, SDIs would have only referred to mini one-piece implants to support an overdenture. Now SDIs include one- and 2-piece implants, offering choices for both removable and fixed prosthetic options. SDIs can be broken up into 2 categories: the mini dental implants (MDIs) that range from 1.8 mm to 2.5 mm in width and 10 mm to 18 mm in length, and the SDIs ranging from 2.5 mm to less than 3.5 mm in width and 12.0 mm to 18.0 mm in length. The US Food and Drug Administration (FDA) gave 510(k) approval for MDIs, and approval for certain brands can be found on fda.gov. The FDA approval of certain MDI brands is “for use as a self-tapping titanium screw for transitional or intrabony long-term applications.” The MDIs are also indicated, according to the FDA website, for “long-term maxillary and mandibular tissue-supported denture stabilization.” SDIs also have FDA 510(k) approval. According to the FDA website, the 510(k) clearance for 3.0 mm-diameter-sized implants is stated as the following:
1. An artificial root structure for single-tooth replacement of mandibular central and lateral incisors and maxillary lateral incisors. The SDI may be immediately restored with a temporary prosthesis that is not in functional occlusion.
2. When splinted together as an artificial root structure for multiple-tooth replacement of mandibular incisors. The SDI may be restored after a period of time or placed in immediate function.
3. For denture stabilization using multiple im¬plants in the anterior mandible and maxilla. The SDIs may be restored after a period of time or placed in immediate function. It is apparent that there are approved indicated uses for dental implants in this size range. These FDA statements are only guidelines for the dental practitioner, and a clinician must make the final decision for his or her patient. Under the appropriate clinical conditions, both MDIs and SDIs have a definitive place in dental implant treatment planning. When a clinician is formulating a treatment plan to replace missing teeth, spacing of dental implants is a high priority consideration. Implant spacing impacts issues such as number of implants and the proximal bone vascularity. If implants are closer than 2.0 to 3.0 mm, the propensity for bone loss increases, which in turn can create aesthetic issues through soft-tissue loss. Spacing implants too close together can even affect their survival rate. Previously, when the multitude of SDIs was not available, spacing issues were not as easily or adequately resolved by the clinician. Having the option of smaller diameter implants allows for more treatment planning choices as far as spacing issues. The option of different sizes also allows for creativity in treatment planning, with clinicians often combining traditional-sized implants with SDIs. For the last 5 years or so, SDIs have been available as a 2-piece option. This has completely changed the scope of treatment planning options in a positive manner. There are advantages and disadvantages to one-piece implants. One advantage is the fact that there is not a micro¬gap between the implant and the abutment, which (according to Dr. Carl Misch) allows for a closer proximity between implants and teeth. The disadvantages of one-piece implants, in general, are related to provisionalization and the need for more exact implant placement with respect to angles. If provisionalizing one-piece implants for less than a full-arch case, the implants should be out of occlusion during the healing period. If one-piece implants are used for a full-arch case, then the implants need to be splinted. The angulation of the implant is an issue for every one-piece implant, as angle correction abutments are not available. When a one-piece implant is used to support an overdenture, the patient is committing to the overdenture option. This long-term commitment is one that must be emphasized to the patient. The surface area of the implant that contacts bone is a consideration of SDIs. With less surface area contacting the bone, the clinician should consider the loading forces on the implants with regard to the patient’s occlusal forces. The patient’s existing height or width of bone also relates to the forces on a dental implant. If there is an increased cantilever due to a lower bone height, this should be taken into consideration. A clinician’s choice to use longer implants, more implants, and implants with increased surface texture are all ways to reduce the forces on implants. The emergence profile must be considered when treatment planning, especially in the aesthetic zone. If the diameter of an implant is too narrow, then the emergence profile will be too extreme, creating the possibility of hygiene and aesthetic issues. This is especially evident with one-piece dental implants. The multitude of width options from manufacturers and the use of a custom abutment help to negate this issue. It is important for a clinician to be knowledgeable of the manufacturers’ offered options for the various implant systems, as this directly pertains to ideal treatment for a patient. For instance, some manufacturers don’t make multiunit angle-correcting abutments for certain SDIs, which could be an issue for certain implant cases. The ramifications of a manufacturer’s inclusion of parts could also affect issues such as whether digital scans can be taken, if angled abutments are available, or if various healing cap sizes are available for the treatment planned SDI. Gaining in-depth knowledge of a manufacturer’s available parts is an important pretreatment step, especially with SDIs, as there are less parts made for this segment of the market, in general. In this
88 MDI ClinicalStudies from AroundTheWorld
Malmo, Sweden 2014
The effect of implant diameter on osseointegration utilizing simplified drilling protocols.
Jimbo R, et al. Clin Oral Implants Res. 2014.
Authors
Jimbo R1, Janal MN2, Marin C3, Giro G4, Tovar N4
Department of Prosthodontics, Faculty of Odontology, Malmö University, Malmö, Sweden.
2
Department of Epidemiology and Health Promotion, New York University, New York, NY, USA.
3
Department of Dentistry, Division of Oral and Maxillofacial Surgery, Universidade Federal de Santa Catarina, Brazil.
4
Department of Biomaterials and Biomimetics, New York University, New York, NY, USA.
Citation
Clin Oral Implants Res. 2014 Nov;25(11):1295-1300. doi: 10.1111/clr.12268. Epub 2013 Oct 8.
Abstract
OBJECTIVES: To observe and to compare histologically and histomorphometrically, the combined effect of drilling sequence and implant diameter in vivo.
MATERIAL AND METHODS: A total of 72 alumina-blasted and acid-etched Ti-6Al-4V implants with three different diameters (3.75, 4.2, and 5 mm, n = 24 for each group) were placed in the right and left tibiae of 12 beagle dogs. Within the same diameter group, half of the implants were inserted after a simplified drilling procedure (pilot drill + final diameter drill) on one tibia and the other half were placed using the conventional drilling procedure on the other tibia. After 1 week, half of the animals (n = 6) were sacrificed, and the other half was sacrificed after 5 weeks (n = 6). The retrieved bone-implant samples were subjected to non-decalcified histologic sectioning, and the bone-to-implant contact (BIC) and the bone area fraction occupancy (BAFO) were analyzed. Primary statistical analysis used a mixed model analysis of variance with significance level set at P < 0.05.
RESULTS: Histologic observation showed that at 1 week, immature woven bone formed in vicinity of the implant, whereas at 5 weeks, the woven bone was replaced by lamellar bone, which formed in proximity with the implant. Histomorphometrically, the simplified technique was associated with significantly greater BIC and BAFO after 1 week. Differences between techniques were not longer apparent after 5 weeks, but BAFO was inversely and significantly associated with implant diameter at that time.
CONCLUSIONS: The simplified technique did not impair either early or late bone formation for any tested implant diameter; however, WIDER diameters were associated with LESS bone formation at longer healing times for both techniques.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd.
89 MDI ClinicalStudies from AroundTheUSA
New York,NY 20 13
The effect of simplifying dental implant drilling sequence on osseointegration: an experimental study in dogs.
Giro G, et al. Int J Biomater. 2013.
Authors
Giro G1, Tovar N, Marin C, Bonfante EA, Jimbo R, Suzuki M, Janal MN, Coelho PG.
Author information
1
Department of Biomaterials and Biomimetics, New York University, 345E 24th Street, Room 813A, New York, NY 10010, USA.
Citation
Int J Biomater.
2013 Jan 30.
Abstract
OBJECTIVES: To test the hypothesis that there would be no differences in osseointegration by reducing the number of drills for site preparation relative to conventional drilling sequence.
METHODS: Seventy-two implants were bilaterally placed in the tibia of 18 beagle dogs and remained for 1, 3, and 5 weeks. Thirty-six implants were 3.75 mm in diameter and the other 36 were 4.2 mm. Half of the implants of each diameter were placed under a simplified technique (pilot drill + final diameter drill) and the other half were placed under conventional drilling where multiple drills of increasing diameter were utilized. After euthanisation, the bone-implant samples were processed and referred to histological analysis. Bone-to-implant contact (BIC) and bone-area-fraction occupancy (BAFO) were assessed. Statistical analyses were performed by GLM ANOVA at 95% level of significance considering implant diameter, time in vivo, and drilling procedure as independent variables and BIC and BAFO as the dependent variables.
RESULTS: Both techniques led to implant integration. No differences in BIC and BAFO were observed between drilling procedures as time elapsed in vivo.
CONCLUSIONS:
The simplified drilling protocol presented comparable osseointegration outcomes to the conventional protocol, which proved the initial hypothesis.
90 MDI ClinicalStudies from AroundTheWorld
Tamil Nadu, India 2012
Narrow diameter implant in posterior region
J Indian Soc Periodontol. 2012 Oct-Dec; 16(4): 610–613.
Jumshad B. Mohamed, Md. Nazish Alam, Arif Salman, and S. C. Chandrasekaran
Department of Periodontics and Implantology, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India
Abstract
Dental implants placement can sometimes be limited due to physical conditions, wherein the horizontal space is limited by adjacent teeth and roots or situations in which there is narrow alveolar ridge, By using a narrow diameter implant (NDI), the need for bone augmentation can be avoided. In situations where there is limited horizontal space, a NDI may be the only option to replace a missing tooth.
91 MDI ClinicalStudies from AroundTheWorld
Bern, Switzerland2004
Clinical evaluation of small-diameter ITI implants: a prospective study.
Zinsli B, et al. Int J Oral Maxillofac Implants. 2004
Jan-Feb.
Authors
Zinsli B1, Sägesser T, Mericske E, Mericske-Stern R.
Author information
1
Department of Prosthodontics, University of Bern, School of Dental Medicine, Bern, Switzerland.
Citation
Int J Oral Maxillofac Implants. 2004 Jan-Feb;19(1):92-9.
Abstract
PURPOSE: Dental implants with a reduced diameter are designed for specific clinical situations, such as placement of implants where bone width is narrow or between adjacent teeth that have only a narrow space between them. They are particularly useful when replacing small teeth such as lateral maxillary and mandibular incisors. The aim of the present study was the clinical evaluation of 2-part ITI implants (full-body screws with a 3.3-mm diameter).
MATERIALS AND METHODS: One hundred forty-nine partially or completely edentulous patients received a total of 298 2-part ITI implants over a 10-year period. After a standard healing period (3 to 6 months), the implants were restored with fixed restorations such as single crowns or fixed partial or complete prostheses or overdentures. Complete prosthesis or overdenture in the edentulous jaw was the predominant type of restoration. All patients followed a strict maintenance program, with regular recalls at least once a year. The survival rate of the implants was analyzed, and prosthetic complications were assessed.
RESULTS: Three implants were lost during the healing phase on account of peri-implant infection. Two implant body fractures with an osseous length of 8 mm were observed (one after 2 years of observation, the other after 6 years). Four implants exhibited transient peri-implant inflammation that was treated successfully by interceptive therapy. The cumulative 5-year survival rate of the implants was 98.7% (96.6% after 6 years). Prosthetic complications were mostly limited to loose occlusal screws and sore spots caused by the denture base.
DISCUSSION: Within the limited observation period, failures of small-diameter implants were infrequent. Prosthetic complications were not dependent on the use of small-diameter implants.
CONCLUSION:
The use of 3.3-mm ITI implants appears to be predictable if clinical guidelines are followed and appropriate prosthetic restorations are provided. However, fatigue fracture may occur after a long period of function.
92 MDI ClinicalStudies from AroundTheWorld
Cairo,Egypt 2017
Peri-implant biomechanical responses to standard, short-wide, and double mini implants replacing missing molar supporting hybrid ceramic or full-metal crowns under axial and off-axial loading: an in vitro study.
Elfadaly LS, et al. Int J Implant Dent. 2017.
https://www.ncbi
.nlm.nih.gov/pmc/
articles/PMC5515718/
Elfadaly LS1, Khairallah LS2, Al Agroudy MA2.
Author information
1
Fixed Prosthodontics, Cairo University, Giza, Egypt. dr.l.fadaly@gmail.com.
2
Fixed Prosthodontics, Cairo University, Giza, Egypt.
Citation
Int J Implant Dent. 2017 Dec;3(1):31. doi: 10.1186/s40729-017-0094-2. Epub 2017 Jul 13.
Abstract
BACKGROUND: The aim of this study was to evaluate the biomechanical response of the peri-implant bone to standard, short-wide, and double mini implants replacing missing molar supporting either hybrid ceramic crowns (Lava Ultimate restorative) or full-metal crowns under two different loading conditions (axial and off-axial loading) using strain gauge analysis.
METHODS: Three single-molar implant designs, (1) single, 3.8-mm (regular) diameter implant, (2) single, 5.8-mm (wide) diameter implant, and (3) two 2.5-mm diameter (double) implants connected through a single-molar crown, were embedded in epoxy resin by the aid of a surveyor to ensure their parallelism. Each implant supported full-metal crowns made of Ni-Cr alloy and hybrid ceramic with standardized dimensions. Epoxy resin casts were prepared to receive 4 strain gauges around each implant design, on the buccal, lingual, mesial, and distal surfaces. Results were analyzed statistically.
RESULTS: Results showed that implant design has statistically significant effect on peri-implant microstrains, where the standard implant showed the highest mean microstrain values followed by double mini implants, while the short-wide implant showed the lowest mean microstrain values. Concerning the superstructure material, implants supporting Lava Ultimate crowns had statistically significant higher mean microstrain values than those supporting full-metal crowns. Concerning the load direction, off-axial loading caused uneven distribution of load with statistically significant higher microstrain values on the site of off-axial loading (distal surface) than the axial loading.
Results
Effect of implant design on peri-implant microstrains
Results revealed that standard implant showed the statistically significantly highest mean microstrain values (3362.4 ± 757.4 μɛ). Double mini implant showed statistically significantly lower mean microstrain values (801.6 ± 251.4 μɛ), while short-wide implant showed the statistically significantly lowest mean microstrain values (697.6 ± 79.7 μɛ), with a P value <0.001 (Table 1).
CONCLUSIONS:
Implant design, superstructure material, and load direction significantly affect peri-implant microstrains.
Conclusions
Within the limitations of this in vitro study, the following conclusions could be drawn:
1. Implant design, superstructure material, and load direction significantly affect peri-implant microstrains.
2. The recorded compressive and tensile microstrains for the tested designs were within the physiologic loading range, as they did not exceed the compressive or tensile strength of the bone-implant interface, which is more than 3000 microstrains except for the standard sized implant supporting Lava Ultimate crowns under both loading directions.
3 .Off-axial loading leads to uneven distribution of loads, in standard diameter implant, due to the cantilever effect, which caused microstrain values exceeding the physiologic limit, thus causing clinical failure over time.
4.Use of splinted double mini implants and short-wide implant to restore missing mandibular molar reduces cantilever effect which leads to lowering of peri-implant microstrains under off-axial loading.
5.Usage of full-metal crown implant superstructure reduces the peri-implant microstrain values compared to using Lava Ultimate crowns.
According to Misch [23], a solid implant with a 1.23-mm diameter has the same resistance to bending fracture as the annulus region of a 3.75-mm traditional design. Moreover, a solid 3-mm implant has an approximately 340% increase in moment of inertia over the 3.75-mm traditional two-piece root form at the annulus position.
According to Kheiralla and Younis [12], off-axial loading of single mini implant (3-mm diameter) supporting single molar crown induced mean microstrains value higher than the physiologic limit
while in this study, the mean microstrain value of double mini implant supporting metal and Lava Ultimate crowns under off-axial loading were within the physiologic limit (890.8 μɛ and 1137.6 μɛ, respectively).This is in accordance with Balshi et al. [38] who stated that two implants can basically eliminate MD bending and that this situation can enable double implants to induce even less load magnification than a wide diameter implant.
In this study, although short-wide implants showed mean peri-implant microstrains under axial loading higher than off-axial loading, axial loading of short-wide implant resulted in compression microstrains in all surfaces in case of metal and lava ultimate crowns, indicating that microstrains were distributed almost equally on all surfaces under both axial and off-axial loading. In this study, it was noticed that short-wide implant showed lowest off-axial loading in comparison with standard and double mini implants.
93 MDI ClinicalStudies from AroundTheUSA
Utica,NY 2013
Small-Diameter Implants:
A Treatment Consideration for the Maxillary Edentulous Patient 2013
Brian J. Jackson, DDS
DentistryToday
https://www.dentalce
today.com/courses/136
%2FPDF%2FDT_Nov_13
_167_fnl.pdf
INTRODUCTION
Small-diameter implants (SDIs) appeared in the discipline of implant dentistry as retainers for a transitional prosthesis while conventional sized endosseous implants osseointegrated. Recent FDA approval of SDIs for long- term use has broadened their indications. The incorporation of SDIs for the treatment of the maxillary edentulous patient with atrophic alveolar bone and large pneumatized sinuses has demonstrated successful outcomes. The SDI protocol for the edentulous maxilla is implant placement anterior to the sinus with delayed loading of the complete maxillary overdenture. This article and the case report presented demonstrate the use of SDIs to assist in the retention and stability of a maxillary complete overdenture. Implant dentistry has become a major aspect of clinical dental practice due to the biological concept of osseointegration. Although conventional size endosseous implants received FDA approval in 1970, SDIs have recently gained similar approval.1
In 2004, the FDA approved SDIs for long-term use for full and partial denture stabilization as well as fixed multiunit prostheses.
This approval applies to implants less than 3 mm in diameter, and more specifically, 1.8 mm, 2.1 mm, and 2.4 mm, and corresponding lengths greater than 10 mm. The applications of SDIs for increased stability and retention of overdentures have demonstrated successful clinical outcomes. As a result, the indications for SDIs for long-term use have gained wider acceptance and interest. Although the mandibular complete denture patient has experienced the majority of clinical limitations, the maxillary edentulous condition demonstrates a similar compromised state in regards to form and function. The demand for complete removable dentures will continue to increase as the United States edentulous population approaches 40 million.2 The incorporation of SDIs to aid in stability and retention for the maxillary complete denture patient can enhance speech, function, aesthetics, and comfort.3
Most importantly, dental implants retard the rate of alveolar bone resorption in the maxilla.4,5
As a result, the SDI-retained maxillary overdenture can achieve patient expectations and demonstrate excellent treatment outcomes. The SDI design, as well as the surgical and prosthetic protocol, possesses various characteristics for a successful treatment plan for the edentulous maxilla. The one-piece, small-diameter (2.4 mm) design possesses strength while engaging the atrophic cortical alveolar ridge and underlying cancellous bone (Figure 1).
The strength of the SDI is associated with the one-piece design and the material nature of the titanium alloy (Ti-6AI-4V) structure.
The surgical protocol consisting of a flapless, partial osteotomy approach simplifies the procedure and risks for the general or medically compromised patient. The prosthetic stage can be initiated as an immediate load or under traditional stage protocols, depending on biomechanics as it relates to the quality and quantity of bone.
This minimally invasive approach unique with SDIs parallels other such trends in healthcare services.6
The case presented in this paper demonstrates the utilization of SDIs to retain a maxillary complete overdenture. The treatment plan was approached in a staged manner, including initial extraction with site preservation followed by subsequent implant placement and prosthetic reconstruction. The mandibular arch was treated with conventional, nonimplant dental approaches. The treatment was completed in 13 months with a resultant ideal clinical outcome while achieving patient expectations.
CONCLUSION
The utilization of SDIs has grown in clinical practice since FDA approval for long-term use. The minimally invasive protocol, and reduced treatment times and cost favor the incorporation of this alternative to conventional implants. The usage of SDIs to aid in retention of the overdenture patient should be a treatment consideration for the edentulous maxilla. Although the current body of evidence is promising, the need for long-term studies is essential for widespread acceptance by the dental profession.
94 MDI ClinicalStudies from AroundTheUSA
Pittsburgh,P a 2006
USE OF MINI IMPLANTS FOR REPLACEMENT AND IMMEDIATE LOADING OF 2 SINGLE-TOOTH RESTORATIONS:
A CLINICAL CASE REPORT 2006
Azfar A. Siddiqui, DMD, MSc
Mark Sosovicka, DMD
Mark Goetz, CDT
Department of Maxillofacial Prosthetics
School of Dental Medicine at the University of Pittsburgh, Pa
Journal of Oral Implantology 83
Vol. XXXII/No. Two/2006
http://www.joionline
.org/doi/pdf/10.1563/
794.1?code=AAID-Pre
mDev
Numerous long-term studies have shown that treatment with dental implants can provide edentulous patients with a more stable alternative to complete dentures and partially edentulous patients with a more conservative form of tooth replacement than conven- tional fixed partial dentures. Until recently, commercially available dental implants have been limited to diameters ranging from 3.0 mm to 7.0 mm. Although this range of diameters has been able to address most clinical needs, partially edentulous patients who could not accommodate a 3.0-mm-diameter implant without damaging adjacent dental structures were excluded from implant therapy. This article reports on the surgical treatment and immediate restoration of a patient who received mini implants that were 2.4 mm in diameter.
INTRODUCTION
Endosseous dental-implant rehabilitation can provide partially or completely eden- tulous patients with function and es- thetics similar to natural denti- tion while preserving adjacent teeth.1–3 In clinical situations where residual dentitions are healthy and there are no systemic contraindications, dental-implant therapy may represent the high- est standard of care for tooth replacement. Commercially available dental implants generally range in di- ameter from 3 mm (ie, ”narrow diameter”) to 7 mm (ie, ”wide body,” ”wide diameter ”), with the vast majority of implants falling in the ”standard diameter ” range of 3.7 mm to 4.0 mm.4 When placing dental implants in par- tially edentulous patients, it has been recommended to maintain 2 mm to 3 mm of available space between the surface of the im- plant and the residual dentition to avoid impinging or damaging the periodontal ligaments of the adjacent teeth.5 Unfortunately, some patients have been tradi- tionally excluded from the bene- fits of implant therapy because they lacked adequate mesiodistal edentulous space to accommo- date even a narrow-diameter implant. Implants with diameters ��2.7 mm (ie, ”mini implants”) were initially developed for placement in conjunction with standard- diameter implants to stabilize and retain an interim prosthesis during the healing phase.4,6–8
Other research has suggested that the pull-out strength of endosseous implants may be based on the length rather than the diameter of the implant,9 and histologic analysis has shown that mini implants undergo osseo- integration
COMPARABLE to that of larger-diameter implants.10
These findings have led some clinicians to advocate the use of mini implants to support and/or retain definitive prostheses.11–13 This article reports on the clinical use of mini implants in a patient with congenitally missing mandibular canines with limited mesiodistal bone dimension.
CONCLUSIONS
Mini implants are indicated for areas where the use of narrow- diameter implants (3.0 mm) are contraindicated. Until long-term longitudinal clinical data on mini dental implants are available, their use should be limited to areas with potentially less occlu- sal load.
95 MDI ClinicalStudies from AroundTheUSA
New York,NY 2014
Immediate Dental Implant Placement: Technique, Part 1
Authored by
Dr Gary Greenstein, DDS, MS, professor department of periodontology College of Dental Medicine, Columbia University, New York, NY.
Dr. Cavallaro clinical associate professor Columbia University, NY
https://www.dental
cetoday.com/courses
/145%2FPDF%2FDT_
Jan_14_169_fnl.pdf
INTRODUCTION
Immediate dental implant placement refers to insertion of an implant directly after a tooth is extracted, whereas delayed positioning occurs at some later time. The concept of placing implants immediately after tooth removal was introduced in the 1970s.1 Currently, widespread acceptance of this procedure is due to its high survival rate.2,3 However, placement of immediate implants in different regions of the mouth and under diverse conditions can be challenging. This 2-part article addresses issues relevant to immediate implants (part 1), and provides practical clinical information for positioning immediate implants in different sections of the mouth (part 2).
BACKGROUND INFORMATION
Classification of Extraction Sockets
The following classification system identifies clinical scenarios related to immediate implant placement4 (classification of socket type is dependent on information obtained with a periodontal probe, visual, and radiographic assessments): l Type I: The bony socket is intact, and the soft-tissue form is undisturbed.
l Type II: The bony socket is intact in the coronal aspect of the socket, but a fenestration is present in the apical area. The soft tissue remains intact and undisturbed.
l Type III: Bone loss is present in the coronal aspect of the socket. The soft tissue remains intact and undisturbed.
l Type IV: Bony defects exist in conjunction with soft- tissue deformity.
Indications and Contraindications for Immediate Implant Placement
There are a series of decisions that need to be made prior to proceeding with immediate implant placement. First, the socket type needs to be assessed and categorized as shown above. Type I and usually Type II (depending on extent of the defect) sockets are candidates for immediate implant placement and require preservation of adjacent tissues around an immediate implant. Types III and IV sockets frequently warrant delayed placement and soft- or hard- tissue augmentation prior to implant insertion. This paper mainly focuses on surgical management of Type I cases.
Management of cases (immediate versus delayed implant placement) requires both a surgical and prosthetic perspective. Prior to initiating therapy, a patient should be de- fined as having a high or low risk of attaining an excellent esthetic result, especially in the esthetic zone. Table 1 outlines critical determinants for evaluating patients.5 The main advantages of immediate implant placement are that they save time and there are fewer patient visits. There are numerous indications for tooth replacement with an immediate implant when an adequate amount of bone and soft tissue are available to support it: deciduous tooth, endodontic failure, caries, deep probing depths due to periodontitis, vertical root fracture, and idiopathic root resorption. Contradictions to inserting immediate implants include inadequate height or width of bone, lack of soft tissue, adverse location of nerves, proximity of adjacent teeth, failure to achieve primary stability, and inability to attain a restoratively reasonable position, angulation or sink depth of the implant.
Closing Remarks
Placement of immediate implants is a predictable procedure and attention to detail is essential to ensure success when placing these implants. Type 1 and usually Type 2 sockets are candidates for immediate implant placement and require preservation of adjacent tissues around the implant. Part 1 of this article has discussed indications/contraindications for immediate implant place- ment, healing phase and bone loss after extraction, and practical suggestions for immediate implant placement. Part 2 will provide practical information for positioning immediate implants in different sections of the mouth.
96 MDI ClinicalStudies from AroundTheUSA
New York,NY 2014
Immediate Dental Implant Placement: Technique, Part 2
Authored by
Dr Gary Greenstein, DDS, MS, professor department of periodontology College of Dental Medicine, Columbia University, New York, NY.
Dr. Cavallaro clinical associate professor Columbia University, NY
https://www.dental
cetoday.com/courses
/149%2FPDF%2FDT
_feb_14_170_fnl.pdf
INTRODUCTION
Immediate dental implant placement, whereby the implant is inserted directly after a tooth is extracted, has gained widespread acceptance based on a high survival rate.1,2 However, placement of immediate implants in different regions of the mouth and under diverse conditions can be challenging. Part one of this 2-part article addressed important clinical issues relevant to immediate implants. Part 2 provides practical clinical information for positioning immediate implants in different sections of the mouth, with a focus on Type 1 extraction sockets.
POSITIONING IMMEDIATE IMPLANTS BY REGIONS OF THE MOUTH
Jumping Distance
The jumping distance is a term that refers to the gap between an immediately placed implant and the bone’s ability to bridge the gap.3 Usually, if the gap is less than 2.0 mm, it will fill with bone without bone grafting.4,5-7 Others suggest that an even greater distance can heal without any osseous augmentation.8,9 Maxillary Anterior Teeth—An osteotomy is created on the palatal aspect of the socket (Figures 1a to 1e). It is advisable to take a side cutting (Lindemann) drill and create a ledge in the palatal bone two thirds the distance from the crest of bone to the apex. This ledge is used as a purchase point to place twist drills. It may be useful to enter the bone at an angle with a twist drill and then straighten it up as the osteotomy is created. Ideally, the implant will be positioned so that incisal edges of the mandibular teeth are aiming at the cingulum of the future anterior restoration. Maxillary teeth protrude at about 110°; thus it is necessary to drill the osteotomy in a manner that positions the implant to restore the desired tooth position and contour. It is advisable to keep the implant slightly lingual in the socket and it should not touch the buccal plate of bone. The horizontal biologic influence of the implant should be respected to avoid inducing buccal alveolar bone loss.10 As previously indicated, implants should be placed one mm subcrestally as viewed from the labial osseous crest. In addition, to avoid an implant being pushed buccally upon insertion, it is a good idea to reshape (remove) a small amount of palatal bone at the crest prior to implant placement. Maxillary Bicuspids—In the first bicuspid site, if the furcation bone interferes with selecting an ideal osteotomy location, it should be removed. If the furcation bone is thick, then the osteotomy can be initiated there. Usually, the buccal socket of a 2-rooted bicuspid is not a good location for an implant. It is too far to the buccal, and often there is a labial concavity of the alveolus. Thus, this location should be avoided because it will provide poor esthetics, and drilling an osteotomy in this site can result in labial plate perforation. The osteotomy should be drilled relatively straight and the implant should be directed at the buccal aspect of the lingual cusp of the opposing arch. Occasionally, the palatal root of a 2-rooted premolar is in a favorable location (relative to adjacent teeth) to be used as a site for osteotomy preparation and implant insertion (Figures 2a to 2c). The clinician must recall that as the position (mesiodistal and bucco- lingual location that the im- plant’s platform occupies within the bone) deviates from the center of the tooth to be restored, then additional sink depth to provide for running room to create a proper emergence profile of the restoration must be created. Maxillary Molars—The osteotomy should be drilled in the furcation bone, and when inserted, the implant may be totally or partially surrounded by bone. As long as primary stability is attained, the socket will fill with bone and the implant will integrate circumferentially. Sometimes it is necessary to use a large-diameter implant to attain mechanical retention against the buccal—palatal or mesial—distal aspects of the alveolus. Other times, the furcation bone is not adequate in subantral height for a dental implant, and a transcrestal sinus floor elevation needs to be performed. In unusual situations
CONCLUDING REMARKS
Placement of immediate implants is a predictable procedure, and attention to detail is essential to ensure success. The Table20-30 lists guidelines to enhance successful placement of immediate implants in Type I sockets. Management of atypical situations outlined in this paper should enhance results and help avoid esthetic problems. Often, sockets, adjacent or opposing teeth can provide adequate visual cues for implant placement. However, surgical guides can be used to facilitate precise placement of implants.31 This is particularly true if multiple implants are placed or deviations from optimal anatomy are apparent. In this regard, contemporary implant planning/anatomy software can greatly simplify these surgical interventions.32-34
97 MDI ClinicalStudies from AroundTheWorld
Beirut,Lebanon 2016
Clinical Study 2016
The Use of Narrow Diameter Implants in the Molar Area
M. Saad,1 A. Assaf,2,3 and E. Gerges4
1Private Practice Limited to Periodontology and Implantology
International Journal of Dentistry
Volume 2016, Article ID 8253090, 8 pages
https://www.hind
awi.com/journals/
ijd/2016/8253090/
Abstract
Implant rehabilitations in the posterior jaw are influenced by many factors such as the condition of the remaining teeth, the force factors related to the patient, the quality of the bone, the maintenance of the hygiene, the limited bone height, the type and extent of edentulism, and the nature of the opposing arch. The gold standard is to place a regular diameter implant (>3.7 mm) or a wide one to replace every missing molar. Unfortunately, due to horizontal bone resorption, this option is not possible without lateral bone augmentation. In this situation, narrow diameter implant (NDI < 3.5 mm) could be the alternative to lateral bone augmentation procedures. This paper presents a clinical study where NDIs were used for the replacement of missing molars. They were followed up to 11 years. Special considerations were observed and many parameters were evaluated. NDI could be used to replace missing molar in case of moderate horizontal bone resorption if strict guidelines are respected. Yet, future controlled prospective clinical trials are required to admit their use as scientific evidence.
Conclusion
In case of moderate horizontal bone resorption, NDI may be a reliable option to replace a molar, if the following conditions are satisfied:
1.bone quality type 1, 2, or 3,
2.minimum implant length of 10 mm,
3.implant protective occlusion,
4.implant with appropriate macro- and microgeometry,
5.bone thickness between 5 and
6 mm.
Further observational and randomized controlled studies could provide deeper evidence-based conclusions concerning the use of NDI in the posterior jaws.
98 MDI ClinicalStudies from AroundTheWorld
Chieti-Pescara,Italy 2012
Small-diameter dental implants: 2012
An adjunct for retention, stability, and comfort for the edentulous patient
Antonio ScArAno D.D.S., M.D., Associate Professor, Department of Medical, Oral and Biotechnological Science, University of Chieti-Pescara,
Italy
J Osseointegr 2012;3(4):48-50.
Abstract
Aim Studies have shown that mandibular implant overdentures significantly increase satisfaction and quality of life of edentulous elders. Improved chewing ability appears to have a positive impact on nutritional state. Materials and methods Forty edentulous subjects received four permucosal mini-implants for overdentures in the inter- foramina region of the mandible. Almost all participants were still satisfied with their overdentures. Participant satisfaction concerning retention and stability of the mandibular overdenture was assessed. A micro invasive technique was adopted, without open flap and performed in one chirurgical step; this technique can be used also in the so-called “high- risk” patients (anticoagulant terapy, diabetes, etc). results and conclusion The results suggest that a mandibular overdenture retained by 4 mini-implants may be the best treatment strategy for edentulous people with atrophic ridges. The use of mini-implants is in many cases a good clinical alternative to the use of larger diameter implants, in that they enable to reduce surgical time, bleeding, postoperative discomfort and healing time
Discussion and Conclusion
The need for correcting the patient’s problems with disadvantage as it has less resistance to occlusal forces. Balkin et al. (12) reported that histologically the bone appeared to be integrated to the surface of the mini- implant immediately loaded at the light microscopic level, and the bone appeared to be relatively mature and healthy. Using mini-implants supported overdenture as a definitive method for treating the edentulous is relatively recent and this is why there are not so many articles on the topic. This therapeutic alternative is seen by a large group of authors as indicated especially for the mandibular complete edentulism (13, 14). Mini-implant supported overdenture can be in complete edentulous patients a treatment alternative to both conventional dentures and conventional implant retained overdenture (15, 16). The advantages of this type of treatment derives from the characteristics of this type of implant (small diameter, variable length, O-ring retention system), which adapts better to the particular morphological conditions present in full edentulous patients (17). Also, the implants insertion requires less surgical trauma, this being a beneficial aspect in the context of usually poor general status. This type of treatment has a lower cost compared to conventional implant supported overdenture, by the lower cost of mini- implants, and also due to the use, in general, just of the panoramic radiography as imagistic method (computed tomography is an adjuvant method, but not essential in most cases). Also by eliminating some surgical intervention, we eliminate also their costs. Surgical technique may be performed without incision of the soft tissue. The last one is preferred when possible, due to the smaller surgical trauma. This may represent an important benefit of this technique, if we consider the usually poor general status of these patients. On the other hand, the benefits related to an improved stability, better functionality and adaptation are quickly noticed by the patient and increases their level of satisfaction.
In conclusion, small-diameter implants can be a solution in cases of limited bone thickness or in elderly patients.
99 MDI ClinicalStudies from AroundTheUSA
Oklahoma City, Oklahoma 2005
Multi-clinic evaluation using mini-dental implants for long-term denture stabilization: a preliminary biometric evaluation.
Review article
Bulard RA, et al. Compend Contin Educ Dent. 2005.
Authors
Bulard RA1, Vance JB.
Author information
1
Department of Implantology/Department of Oral Maxillofacial Surgery University of Oklahoma College of Dentistry Oklahoma City, Oklahoma, USA.
Compend Contin Educ Dent. 2005 Dec;26(12):892-7.
https://www.ncbi
.nlm.nih.gov/m/pu
bmed/16389776/
Abstract
Mini-dental implants (approximately 1.8 mm to 2.4 mm in diameter) can provide immediate stabilization of a dental prosthetic appliance after a minimally invasive procedure. Furthermore, mini-implants can be used in cases where traditional implants are impractical, or when a different type of anchorage system is needed. Healing time required for mini-implant placement is typically shorter than that associated with conventional 2-stage implant placement and the accompanying aggressive surgical procedure. The design of mini-implants is such that insertion techniques minimize peri-implant tissue and bone damage. Because of their versatility and ease of insertion, mini-implants have proven useful as transitional stabilizers and as fixtures for long-term prosthesis function. This study of mini-implant successes/failures provides data for a thorough review of long-term mini-implant in vivo performance. A biometric analysis of 1,029 MDI mini-implants”, 5 months to 8 years in vivo, representing 5 clinics, facilitated this study of the MDI as a fixture for long-term prosthesis stabilization. MDI failure rates for stabilization on average were 8.83%.
These analyses establish that the MDI mini-implant system can be implemented for long-term prosthesis stabilization and deliver a consistent level of implant success.
100 MDI ClinicalStudies from AroundTheUSA
Mt Pleasant,SC 2019
Inside Dentistry
October 2010
Volume 6, Issue 9
The Unique Benefits of Mini Dental Implants
This minimally invasive procedure offers numerous possibilities for edentulous patients.
By Joe Gillespie, DDS
Inside Dentistry
October 2010
Volume 6, Issue 9
https://www.aeg
isdentalnetwork.
com/id/2010/10/
the-unique-bene
fits-of-mini-dent
al-implants
The dental profession is beginning to face an incredible challenge. Dental practices are treating the largest population explosion in US history-the children of post-World War II, who are now reaching retirement and have unique dental restorative needs. Dental implants have had a tremendous impact in the dental field and have opened new treatment concepts in restorative dentistry. Statistics show the clear need for implant treatment-69% of adults aged 35 to 44 have lost at least one permanent tooth, while 26% of those 65 and over and 44% of the 75-and-over population are edentulous in both arches.1 The aging population is accelerating the need for implant treatment, and within the coming decades, the number of Americans over 65 will grow to represent more than 20% of the total population.2 Within the implant category, mini dental implants (MDIs) represent a promising treatment that has significant potential for growth. The 3M ESPE MDI mini dental implant system (formerly the IMTEC Sendax MDI System), with implants ranging in diameter from 1.8 mm to 2.9 mm, can be applied successfully to stabilize dentures and in other clinical applications. Mini dental implants were accepted by the FDA in 1997,3 and since then studies have found their survival rates to range from 91.2% to 96.3%.4-6 A recent study that followed more than 2,500 implants found a 5-year survival rate of 94.2%.7 MDI treatment is relatively simple to learn and perform, and the minimally invasive procedure can be quickly completed in a general dentist’s office. If there is insufficient bone to anchor a conventional implant, extensive surgical interventions can sometimes be required to attain adequate bone width, resulting in considerable cost for patients. Alternatively, the cost of the MDI procedure is significantly more affordable, making it an attractive option for many.
Discussion
This case is an excellent demonstration of how MDIs can be a much more suitable and comfortable procedure for osteoporotic patients, and also demonstrates their patient acceptance and success. The mandibular implants in the case presented have been in place for 7 years now, and the maxillary for 2 years, and the patient is amazed and thrilled with her restored function. The author often hears “complaints” from patients after this procedure that they’ve gained 5 pounds, which is treated as good news after seeing so many denture patients lose weight due to the inability to maintain proper nutrition. MDI treatment can be a life-altering process for patients who are “dentally handicapped”-those who have been told they do not have enough bone, have too complicated a medical history, or simply cannot afford root form implants. It is an outstanding adjunct for enhancing a practice and making a significant change in patients’ quality of life. References
101 MDI ClinicalStudies from AroundTheUSA
Lenore,North Coralina
2015
Denture Stabilization With Mini Dental Implants
By Dr Paresh Patel
The International Journal of Clinical Implant Dentistry
Sept-Dec 2015 (1)3;101-104
102 MDI ClinicalStudies from AroundTheWorld
Lenore,North Coralina
Novi Ligure,Italy 2015
Minimally Invasive Implant Therapy in Geriatric Patients Using Small Diameter Implants
103 MDI ClinicalStudies from AroundTheWorld
Novi Ligure ,Italy 2017
Small Diameter Implants (SDIs) in Fixed Restorations:Clinical Cases Considerations During 4 Years Follow-Up 2015
Andrea Mascolo*D.D.S,
Master in Oral Surgery and Odontostomatological Urgency, Expert in Minimally Invasizirconia v ve Procedures, Italy
Andrea Mascolo
Studio Mascolo Independent Center for
Dental Research and Dental Training
Novi Ligure (AL) Italy
Abstract
In recent years, the interest and use of small diameter implants have increased considerably. The probable reasons are the clinical credibility in long term use and its minimally invasive placement protocol. Victor Sendax, a conceptualist and developer of small diameter implants, had identified three patients groups in the 1980’s on which the mini implants offered invaluable performances:
for medically, financially, and anatomically compromised patients.
This paper outlines the clinical experience conducted among 28 patients during a follow-up period of four years. This group is heterogeneous in age, concurrent in systemic conditions and represents the type of a private practice patient whose treatments selected have followed the proposed guidelines for the rational use of small diameter implants.
Conclusion
The clinical experience shows good performance of small diameter implants in fixed solutions; the results are appreciated from clinicians and from patients for the minimal invasive approach and functional standpoint. During the follow-up period we have not registered peri-implant bone resorption; we have noticed healthy gingival remodeling around the implants. The reduced diameter of the abutments helps to secure a favorable remodeling of the soft tissues; the abutment connection is able to seal the perimplant area eliminating micro-leakages. The results achieved in the clinical trial encourage the use of small diameter implants in some clinical situations as example thin bony ridges and or limited interdental spaces, not just in anterior areas as initially proposed from earlier literatures. Some of the important factors for a success are: a clinically considerate patient selection, a planning according to the guidelines, and emphasizing judicious checking on occlusion after restoration is completed.
104 MDI ClinicalStudies from AroundTheWorld
Istanbul ,Turkey 2007
Treatment of a narrow, single tooth edentulous area with mini-dental implants: a clinical report.
Dilek OC, et al. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007.
Dilek OC1, Tezulas E.
Oral Implantology
Faculty of Dentistry,
Yeditepe University,
Istanbul, Turkey. ozkand@yeditepe.edu.tr
Abstract
The narrowing of an extraction site often becomes problematic when attempting to restore the space with a conventional wide-diameter implant. A woman is presented who was treated with a square head, mini-dental implant-supported fixed denture for a maxillary with a narrowed edentulous area, with a mesiodistal width of 5 mm. The implant, with a diameter of 2.4 mm, was inserted without reflecting the mucoperiosteal flap and was loaded immediately. During 12 months of follow-up, there has been no bone resorption and no inflammation observed around the implant.
In conclusion, in terms of both clinical and aesthetic criteria, small diameter, mini-dental implants can be successfully used as an alternative to treatment with FIXED partial dentures.
105 MDI ClinicalStudies from AroundTheWorld
Tehran,Iran 2011
Clinical evaluation of small diameter straumann implants in partially edentulous patients: a 5-year retrospective study.
Yaltirik M, et al. J Dent (Tehran). 2011.
Authors
Yaltirik M1, Gökçen-Röhlig B, Ozer S, Evlioglu G.
Author information
1
Associate Professor, Department of Oral Surgery, Faculty of Dentistry, Istanbul University.
Citation
J Dent (Tehran). 2011 Spring;8(2):75-80. Epub 2011 Jun 30.
Abstract
OBJECTIVE: The aim of the present study was to retrospectively evaluate small-diameter (3.3 mm) Straumann® dental implants placed in the maxilla or the mandible over a period of 5 years in function.
MATERIALS AND METHODS: Twenty-eight partially edentulous patients received a total of 48 implants over a 5-year period. After the standard healing period (3 to 6 months), the implants were restored with single-tooth prostheses or fixed partial dentures. All patients were followed according to a strict maintenance program with regular recalls. The cumulative survival rates of implants were analyzed and prosthetic complications were assessed.
RESULTS: After 5 years of function, one single 10-mm-long implant in the maxillary premolar region was lost because of recurrent peri-implant infection in a female patient. Two single 10-mm-long maxillary implants placed in the posterior region were lost due to body fracture. The cumulative 5-year survival rate of the implants was 93.75 %. The most common prosthetic complication was loosening of the occlusal screw.
CONCLUSION: Within the limited observation period and the number of patients included in this study, it may be concluded that the use of small-diameter implants appears to be predictable if clinical guidelines are followed and appropriate prosthetic restorations are provided. However, it should be noted that fatigue fracture may occur.
106 MDI ClinicalStudies from AroundTheWorld
2018 Kaunas,Lithuania
New approach towards mini dental implants and small-diameter implants: an option for long-term prostheses
Dept of Dental and Maxillary Orthopedics, Faculty of
Odontology, Medical Academy, Lithuanian
University of Health Science, Kaunas, Lithuania
2Faculty of Odontology, Lithuanian University of Health Science, Kaunas, Lithuania
3Kupiskis Primary personal healthcare center, Kupiskis, Lithuania
Alvydas Gleiznys1 – D.D.S., PhD, assoc. prof.
Gediminas Skirbutis1 – D.D.S., assist.
Ali Harb2 – student
Ingrida Barzdziukaite1 – D.D.S., assist
Ieva
CONCLUSIONS
Implants with small diameters are one of the major advancements in dental history; they can be used successfully in a variety of clinical situations. Researches continue to demonstrate the surgical and prosthodontic success of those implants. They offer patients satisfaction due to less surgical time, less postoperative pain and ability of direct loading after surgery with no harm to bone. Also they are more cost effective option, since they can support a denture with a reduced cost. It must be emphasized that the reduced surface implants require correct treatment planning so that the loading force would not cause bone loss or implant failure. Nevertheless, MDI and SDI showed high survival rates, but spe-cial cautions of bone quality and good oral hygiene should be maintained. Due to simplified procedures, this could be a good choice for unexperienced dentists for their first steps in implantology.
107 MDI ClinicalStudies from AroundTheWorld
2017 Suva,Figi
Comparison of patient satisfaction with mini-implant versus standard diameter implant overdentures: a systematic review and meta-analysis of randomized controlled trials
https://www.ncbi.
nlm.nih.gov/pmc/
articles/PMC5494032/
Int J Implant Dent. 2017
Gowri Sivaramakrishnan1 and Kannan Sridharan2
1Department of Oral Health, College of Medicine, Nursing and Health Sciences, Fiji National University, Brown Street, Suva, Fiji
2Department of Pharmacology, Fiji National University, Extension Street, Suva, Fiji
Gowri Sivaramakrishnan, Phone: +679 9090572, Email: moc.liamg@nanhsirkamaravis.irwog.
Conclusion
However, considering the results obtained from available evidence, mini-implants tend to provide good patient satisfaction compared to standard diameter implants when used for implant-supported overdentures. The results of this meta-analysis should be interpreted keeping in the mind the limited availability of data to be included. This paper would serve as a basis for future research comparing mini-implants with standard diameter implants for implant-supported overdentures.
108 MDI ClinicalStudies from AroundTheWorld
2016 Pradesh,India
https://www.ncbi.
nlm.nih.gov/pmc/
articles/PMC5494032/
Replacement of a molar with two narrow-diameter dental implants
Journal of Indian Society of Periodontology 2016
Wolters Kluwer — Medknow Publicationss
Rajeshwari Penmetsa and Katragadda Raja Venkatesh Murthy
Department of Periodontics, GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh, India
Abstract
Dental implants have demonstrated a high degree of success in the restorations of teeth in partially or completely edentulous patients.
However, WHEN the buccolingual width of the edentulous crest is INSUFFICIENT for the placement of standard sized implants…
the use of TWO or MORE smaller diameter implants should be considered to avoid the need for INVASIVE reconstruction techniques such as grafting procedures.
The present case report describes the replacement of a single mandibular first molar with two narrow-diameter implants, in a 41-year- old male patient. No postoperative complications were reported in the 3-year follow-up period. The placement of two narrow-diameter implants replacing a missing mandibular molar could eliminate the mesiodistal bending, double the support capacity in the buccolingual direction, and minimize stress on the implants. Keywords: Edentulous molar space, narrow atrophied ridge, narrow-diameter implants
INTRODUCTION
Evidence suggests that replacement of missing teeth by dental implant restorations is a successful treatment modality. However, an atrophic mandibular edentulous space could pose a significant challenge to successful oral rehabilitation with dental implants due to inadequate buccolingual dimensions. Regular sized dental implants ensure an adequate bone to implant contact. However, narrow edentulous ridges require the use of small-diameter implants to avoid invasive reconstruction techniques.[1] Conventionally, the low rate of complications, in addition to higher long-term success rates make implant restoration a reliable solution to treat the posterior partial edentulism. Sometimes, however, using only one freestanding implant to support a fully functioning molar can be questioned with reference to the possible bending overload situation as well as representing a biomechanical challenge. One way of countering the potential overload in this situation is to direct the occlusal forces to a centric position on the tooth, thus reducing the bending on the implant. Alternately, this situation can be addressed by supporting a single molar with two smaller diameter implants. This can basically eliminate the mesiodistal bending and double the support capacity in the buccolingual direction, with an added advantage that these smaller diameter implants can be placed in narrow deficient ridges.[2] This case report evaluates the clinical outcome of the placement of two narrow-diameter implants replacing a missing mandibular molar.
CASE REPORT
A 41-year-old male patient reported with a chief complaint of a missing lower left back tooth for 6 years. The tooth had been extracted 6 years back owing to extensive carious involvement and a poor endodontic prognosis. The patient was systemically healthy. His periodontal status was stable. Clinical examination [Figure 1] and study model analysis of the edentulous site revealed a mesiodistal dimension of 10 mm and a crown height length of 6 mm. Ridge mapping revealed a buccolingual dimension of 5 mm at the mesiodistal midpoint of the edentulous space. Considering that a minimum of 0.5 mm of bone should be present on each of the buccal and lingual aspects of an implant,[3] the buccolingual width of 5 mm was deemed insufficient for placement of a regular diameter/wide-diameter implant although the mesiodistal envelope for implant placement was sufficient. The patient was not willing to undergo further surgical procedures for ridge augmentation. Hence, a treatment plan was outlined that included the placement of two narrow-diameter implants, so as to obtain sufficient implant bone surface area to compensate for the deficiency in implant diameter.[3] On radiographic examination [Figure 2], the available bone height in the first molar region was found to be 15 mm from the crest of the ridge to mandibular canal region. It was decided to place two narrow single-stage implants of 2.5 mm diameter and 13 mm length each.
Surgical technique
Following a perioral skin preparation with an antiseptic solution and a presurgical rinse with 0.2% chlorhexidine, local anesthesia (2% xylocaine with 1:80,000 adrenaline) was administered at the surgical site. A midcrestal incision was given at the edentulous site, and full thickness mucoperiosteal buccal and palatal flaps were reflected [Figure 3]. Two osteotomy sites of 2 mm diameter were prepared under copious saline irrigation up to a depth of 13 mm using a pilot drill of 2 mm. Two narrow implants (2.5 mm diameter, single stage) were inserted into the osteotomy sites using a hand wrench [Figure 4] parallel to each other and to the adjacent teeth. The mucoperiosteal flaps were then secured with interrupted sutures [Figure 5], and a postoperative radiograph was taken [Figure 6]. Antibiotics (500 mg amoxicillin thrice daily) and analgesics (100 mg aceclofenac twice daily) were prescribed for 5 days postoperatively. The patient was instructed to rinse with 10 ml of 0.2% chlorhexidine mouthwash twice daily for a week. The sutures were removed after 7 days. Elastomeric impressions were taken and an implant supported provisional acrylic crown was fabricated. This was followed by a metal ceramic fixed prosthesis [Figure 7] 4 months after implant surgery. The patient was instructed regarding maintenance of oral hygiene by means of dental floss and interdental brush. The patient was recalled at 1 month, 3 and 6 months postsurgery for clinical and radiographic evaluation of the implant site and assessment of oral hygiene maintenance. The patient has been monitored for the past 3 years at recall visits and has been comfortable with the prosthesis. Radiographic evaluation has indicated a stable periodontal condition with minimal crestal bone loss [Figure 8].
DISCUSSION
Dental implants are intended to replace the missing roots of a tooth. In the case of a molar, a single implant may not achieve the crown root ratio of the original tooth subjecting the implant to increased occlusal forces. Owing to this reason, prosthesis mobility and screw loosening are the most frequent complications associated with single implant molar restorations.[4] Another disadvantage of a wide-diameter implant is that if the implant fails to osseointegrate, a wider implant for replacement may not be available. In addition, many ridges may not have an adequate buccolingual dimension for placement of a wide-diameter implant, as in the present case. In the present case, the primary implant stabilization was achieved immediately following placement of the implants. Considering the narrow buccolingual ridge dimension, two narrow-diameter implants were used to replace a single missing molar. No postoperative complications were reported in the 3-year follow-up period. In the narrower ridge, studies have suggested the placement of two or more narrow-diameter implants when possible, to obtain sufficient implant bone surface area to compensate for the deficiency in the width of the implant.[1,3,5] This mode of treatment provides increased surface area for osseointegration and reduces lateral forces and bending movements that result from the use of single implants. Two implants also eliminate the inherent mesiodistal cantilever and reduce the potential for overload, spreading occlusal loading forces more effectively. It also decreases the rotational forces around the implant axis thus preventing loosening.[6] Balshi et al., 1979 compared the use of two implants to replace single missing molars to the use of a single-standard implant or a wide-diameter implant and found that the use of two implants to replace a single molar provides more surface area for osseointegration and distributes the occlusal forces over a larger area within the bone compared to one wide-diameter implant of the same length.[6] Romeo et al., Olate et al. (2010), Vigolo et al., and Buser et al. (1997) showed a satisfactory success rate using small-diameter implants, similar to that of standard-diameter implants. Chiapasco et al. (2006) concluded that the reported crestal bone loss figures around narrow implants were within the acceptable range.[7] Wolfinger et al., 2011 analyzed retrospectively the survival rate of implants used in pairs to support a single molar crown over a long-term follow-up period of 3–12 years and found that two implants for the replacement of a single molar had a higher survival rate and fewer complications when compared to single implants.[6] Brian (2011) presented a case report where the author used two smaller diameter (3.0 mm × 2 mm) single-stage implants for replacement of the mandibular molar. The author stated that multiple small-diameter implants can increase the long-term prognosis of the prosthesis by increasing surface area and reducing screw loosening.[8] There is a minimal cost difference in placing a regular implant or two narrow-diameter implants. Although it has been demonstrated that the single-implant, single-molar restoration is an ideal treatment protocol, it appears that the use of two implants to replace a single molar provides biomechanical advantages in deficient ridges.
A drawback with two implants, however, is the need for a minimum of 12 mm of mesiodistal space to accommodate both the implants, and this is not always available.
Nevertheless, when using narrow implants, two implants could be used even when the distance between the adjacent teeth are rather limited. The present case report described the feasibility of the replacement of a single mandibular molar by the placement of two narrow-diameter implants. There is, however, a need for further long term studies to confirm the results presented here and reaffirm the predictability of the procedure.
CONCLUSION
Replacing a single missing mandibular molar with two narrow-diameter dental implants might serve as a viable treatment option and a beneficial approach in specific situations.
109 MDI ClinicalStudies from AroundTheWorld
2004 Philadelphia,Penn.
Complications of Mandibular Molar Replacement with a Single Implant:
A Case Report
• Vicki C. Petropoulos, DMD, MS • • Glenn J. Wolfinger, DMD, FACP • • Thomas J. Balshi, DDS, FACP •
© J Can Dent Assoc 2004; 70(4):238–42
This article has been peer reviewed.
CLINICAL PRACTICE
The replacement of a single molar with 1 implant has been shown to be an effective treatment modality in short-term studies;1,2 however,
this presents a biomechanical challenge.
Occlusal forces are greatest in the molar region, leading to possible increased stress on the implant components as well as the surrounding bone.3 The screw joint for a single implant is susceptible to loosening because a torque relative to the implant axis must be counteracted by the screw joint itself.4
One way of controlling this load is to support a single molar replacement with 2 implants.4
The clinical feasibility of using 2 implants to support a molar restoration has been reported previously.5
Case Report
Patient History
A 57-year-old man in excellent health, with no known allergies or sensitivities to medications, presented to Prosthodontics Intermedica (Fort Washington, Pa.) with the chief complaint “my crown and post came off” (Figs. 1a and 1b). He desired an estimate for an implant. In general, the patient sought dental care only when dental emergencies occurred.
© J Can Dent Assoc 2004; 70(4):238–42
This article has been peer reviewed.
Abstract
This case report describes prosthodontic complications resulting from the surgical placement of a single implant and treatment following these complications. Both the surgical and prosthodontic procedures are described for the treatment of a 57-year-old man who had previously received a single implant for the replacement of a missing molar.
Using 2 implants, 1 mesial and 1 distal to the previously placed single implant proved reliable.
A logical treatment solution is to use 2 implants for the replacement of a single molar to avoid prosthodontic complications.
MeSH Key Words: dental implants, single-tooth; dental prosthesis, implant-supported; dental restoration failure; treatment outcome
110 MDI ClinicalStudies from AroundTheWorld
2018 Zagreb,Croatia
Short-term Postoperative Pain and Swelling Associated with Mini and Standard-Size Implants in the Same Patients
Ines Kovačić, Sanja Peršić, Josip Kranjčić, Visar Disha, Ksenija Rener-Sitar, Asja Čelebić
International Journal of Prosthodontics 2018 February 15
1 PhD Student, Department of Prost hodontics, School of Dental Medicine,
Univ of Zagreb, Zagreb, Croatia.
2 Assistant Professor,Dept of Prosthodontics, School of Dental Medicine, University of Zagreb, Zagreb, Croatia.
3 PhD Student, School of Dent al Medic ine, Universit y of Zagreb, Zagreb, Croatia; Private Practice , Pristina, Kosovo.
4 Associate Professor, Depar tment of Prosthodontics, Study of Dental Medicine, Faculty of Medicine, U niversity of Ljubljana, Ljubljana, Slove nia.
5 Professor, Depar tment of Prosthodontics , School of Dental Medicine & Clinical Hospital Centre Zagreb, University of Zagreb, Zagreb, Croatia.
PURPOSE:
To assess short-term postoperative pain and swelling after insertion of mini dental implants (MDI) and standard-size implants (SSI) in the same patients at different times.
MATERIALS AND METHODS:
A convenience sample of 42 patients (22 females, 20 males; 58 to 73 years old) participated. Half of the participants received MDIs first, and the other half received SSIs first. Self-perceived pain and swelling at 1, 3, 5, 7, and 10 days postoperative were assessed using a 0-10 visual analog scale.
Results and Conclusion
Flapless MDI insertion led to
SIGNIFICANTLY LESS
INTENSE PAIN,
LESS INTAKE of ANALAGESICS,
and
ALMOST NO SWELLING…
compared to SSI insertion.
111 MDI ClinicalStudies from AroundTheUSA
2004 Woodstock ,New York
Full-Arch Fixed Prosthetics Supported by Dental Implants and Natural Teeth:
Planning, Provisionalization, Treatment Sequences:
Two Case Examples
Written by Michael Tischler, DDSTuesday, 31 August 2004
When a patient presents with a partially edentulous arch, fixed restoration of the arch supported by dental implants and natural teeth requires proper planning and provisionalization. First, information must be obtained to help plan the case for function and aesthetics. Study models must be articulated so that the present occlusal relationship can be analyzed. Diagnostic wax-ups and intraoral waxups or diagnostic appliances must be utilized to evaluate aesthetics and phonetics.1 A detailed periodontal evaluation should be performed to determine which teeth can be saved for fixed prosthetic support. Radiographs including periapicals, panographs, and CT scans must be taken to evaluate the osseous support for dental implants. Interactive CT scans with radiographic guides offer detailed information with regard to implant placement related to tooth position and aesthetics.2 Once it is determined which teeth can be saved and an overall plan is made for fixed prosthetics, it then must be decided how the case will be provisionalized during the treatment period. Most patients prefer a fixed provisional over a removable one due to stability, aesthetics, and less interference of speech patterns. There are many advantages to a laboratory-processed fixed provisional versus a chairside-produced provisional prosthesis.3 These advantages include improved aesthetics, smoother surface areas, increased strength, and reduced chair time compared to a chairside produced provisional. Patient feedback about the provisional is also an important step in helping guide the final prosthesis toward an ideal aesthetic and functional outcome. When natural teeth cannot support a provisional restoration, either provisional dental implants or immediately loaded dental implants can offer support for a provisional during a healing period.4 The healing period for a full-arch reconstruction can be up to a year if, for instance, bone grafting and periodontal surgery are incorporated into a plan. This article will present 2 case reports that demonstrate the principles of treatment planning, provisionalization, and treatment sequences to restore a fixed full-arch prosthesis supported by dental implants and natural teeth.
CASE REPORT NO. 1
Figure 1. Clinical view of Case Report No. 1 showing edentulous area of teeth Nos. 6 to 11.
Figure 2. Panograph of Case Report No. 1 showing edentulous areas. A 57-year-old female presented with the chief complaint of inability to wear a removable partial denture. She was missing teeth Nos. 1, 16, 5 to 13, 20, and 29 to 32. An examination revealed moderate to advanced bone loss on her remaining maxillary and mandibular teeth, with no mobility noted (Figures 1 and 2). The patient’s health history was unremarkable.
Figure 3. Chairside wax-up to check relationship of teeth to lip line.
Figure 4. Laboratory-processed provisionals in place, offering ideal lip support and phonetics.
Figure 5. Occlusal view of 2 transitional implants to support provisional prosthesis.
Figure 6. Radiographic guide stent for CT scan positioning.
Figure 7. 3-D view from Sim Plant interactive CT program, showing implants in correct position and angulation.
Figure 8. Panograph view from Sim Plant interactive CT program showing implants in relationship to tooth position.
Figure 9. Surgical guide stent with 2-mm guide pins produced from Sim Plant interactive CT program.
Figure 10. Panograph showing 4 BioHorizons implants and 2 provisional implants. (Note wire- reinforced provisionals on panograph). The first step in determining a treatment plan was to place wax in the position of teeth Nos. 5 to 13 to observe upper lip support (Figure 3). Next, a laboratory-processed roundhouse provisional was created, supported by 2 provisional implants (Figures 4 and 5). It was then necessary to determine if bone grafting would be needed to support dental implants. A radiographic guide stent (Implant Logic Systems) was made to fit over the prepared teeth and fill the edentulous space of teeth Nos. 5 to 13 (Figure 6). This radiographic stent would be placed for the CT scan to allow planning of the dental implants in relation to the final desired tooth position. The patient was then sent for a CT scan, and the information was transferred to Sim Plant (Materiallese), an interactive CT scan program (Figures 7 and 8). The Sim Plant information revealed that some grafting would be performed simultaneous with implant placement. Dental implants were planned in the Sim Plant program in the right and left cuspid and lateral incisor positions. The transitional im-plants (Intra-Lock System) can be seen on the CT scan. These transitional implants would be removed at a later date, prior to final prosthesis delivery. A surgical guide stent with 2-mm guide pins was created by Implant Logic Systems, based on the data planned in Sim Plant (Figure 9). At surgery, 4 BioHorizons (BioHorizons Inc) dental im-plants were placed in position Nos. 6, 7, 10, 11 (Figure 10).
igure 11. Final panograph showing fixed maxillary and mandibular prosthetics.
Figure 12. Clinical view of final fixed prosthetics.
The panograph also reveals the wire-reinforced lab-processed provisionals. During the 5-month period while the implants osteointegrated, periodontal therapy was performed on the remainder of the mouth. After 5 months, the provisional implants were removed, and permanent fixed prostheses were created for the maxillary and mandibular arches (Figures 11 and 12). The implants were splinted separate from the natural teeth with a distal cantilever in the No. 12 position. A mesial cantilever from tooth No.13 was attached to tooth No.14. As planned, pink porcelain was placed at the gingival level, allow-ing only minimal exposure with the patient’s low lip line. The end result was fixed prosthetics supported by dental implants and natural dentition. The patient was satisfied by having her removable partial denture replaced, with improved aesthetics, function, and phonetics.
CASE REPORT NO. 2
Figure 13. Clinical view of Case Report No. 2 showing edentulous area of teeth Nos. 7 to 10 and root tips of teeth Nos. 6 and 11.
Figure 14. Panograph of Case Report No. 2 showing failing anterior bridge and bite collapse.
Figure 15. Clinical view of collapsed bite due to lack of posterior support.
A 48-year-old female in good health presented with a failing fixed prosthesis from teeth Nos. 6 to 11 (Figure 13). Teeth Nos. 6 and 11 were broken off at the gum line and the bridge was removable by hand. The panograph revealed multiple endodontically treated teeth and a severe upward curve to the preexisting anterior bridge (Figure 14). The missing posterior teeth and severe bite collapse likely caused the failure of the present anterior bridge (Figure 15). The remaining teeth were all periodontally stable and would be used to support fixed provisional prostheses.
Figure 16. Laboratory-processed provisionals restoring patient’s vertical dimension.
Figure 17. Surgical guide stent based on the tooth position of the laboratory-processed provisional.
The treatment plan consisted of establishing a correct vertical dimension with a fixed implant and natural tooth-supported prostheses. Teeth Nos. 6 and 11 were deemed hopeless and would be removed. The first step was to create a laboratory-processed provisional that would fulfill the goals with respect to vertical occlusal height and aesthetics (Figure 16). Two provisional implants (Intra-Lock System) were placed in the positions of teeth Nos. 6 and 11 to support the provisional prosthesis. Once the fixed provisional was delivered, a surgical stent was created based on the provisional to guide implant placement into the correlating tooth position (Figure 17). BioHorizons (BioHorizons) dental implants were planned in tooth positions 7 to 10 and 13 on the maxilla and 28 to 30 on the mandible.
Figure 18. Panograph showing 4 BioHorizons Implants in teeth positions 7 to 10 and 2 transitional implants supporting the wire-reinforced provisionals. Wire-reinforced provisionals can be seen on mandible.
Figure 19. Clinical view of healed dental implants with healing caps.
The maxillary implants were placed as a 2-stage protocol and left covered by the gingival tissue. The postsurgical panograph shows the 2 provisional implants and the 5 maxillary implants (Figure 18). The mandibular implants were placed at a later date and also left as a 2-stage procedure. After a healing period of 4 months, all implants were uncovered and the tissue was formed with healing caps (Figure 19). Traditional crown and bridge impressions were made, and the metal framework was created on the models.
Figure 20. Clinical view of final porcelain-fused-to-metal fixed prosthesis.
The final prosthesis was delivered a few weeks later (Figure 20). Note how the vertical dimension has been reestablished and full arch stability has been achieved. The provisional implants were removed at the time of permanent crown delivery. The patient has achieved a stable vertical dimension and improved aesthetics supported by both dental implants and natural teeth.
CONCLUSION
The 2 cases presented show the treatment sequences necessary to restore a full arch with fixed prostheses supported by dental implants and natural teeth. The process of diagnostic wax-ups and treatment planning are key steps in determining the final result. Management of provisional replacement utilizing provisional implants is also a key step in transitioning a case. Utilizing these principles of treatment planning and provisionalization, restoration of an arch with dental implants and natural teeth can be rewarding for both the patient and the treating dentist.
References
1. Garcia LT, Bohnenkamp DM. The use of diagnostic wax-ups in treatment planning. Compend Contin Educ Dent. 2003;24(3):210-214.
2. Tischler M. Interactive computerized tomography for dental implants. Treatment planning from the prosthetic end result. Dent Today. 2004;23(3):90-93.
3. Binkley CJ, Irvin PT. Reinforced heat-processed acrylic resin provisional restorations. J Prosthet Dent. 1987;57(6):689-693.
4. Petrungaro PS, Windmiller N. Using transitional implants during the healing phase of implant reconstruction. Gen Dent. 2001;49(1):46-51.
Dr. Tischler maintains a private practice in Woodstock, NY. He is a diplomate of the International Congress of Oral Implantologists and the American Board of Oral Implantology/Implant Dentistry, a fellow of the Misch International Implant Institute, a fellow of the Academy of General Dentistry, and an associate fellow of the American Academy of Implant Dentistry. He can be reached at (845) 679-3706 or visit tischlerdental.com.
112 MDI ClinicalStudies from AroundTheWorld
2011 Meerut, India
Mini Dental Implants-
The Same Day Implants
Puneet Chopra,1 Priyanka Chopra,2 Harpreet Singh Grover3
Meerut, India
2011 Int. Journal of Contemporary Dentistry
ABSTRACT
The computer and medical worlds are both striving to develop smaller and smaller components. In similar fashion, The Mini Dental Implants represents a smaller version of the dental implant. Mini Dental Implants are titanium screws that replace the root of a tooth. The ball shaped head and collar design can be used for both permanently cemented crowns and bridges as well as securing full or partial dentures. When used for fixed or cemented applications the prosthesis is cemented directly to the head of the implant. As a revolutionary departure from routine dental implant methods, Mini Dental Implants are so narrow they are typically inserted directly through the overlying gum tissue and into the bone underneath. Consequently the need to surgically cut and “flap” open the gum tissue, routinely required for standard implant systems, is avoided in most Mini Dental Implant applications. As a result, post-insertion patient irritation and soreness is significantly reduced. It is often possible to provide the complete mini implant service in a single office visit. Because of the unique, minimally invasive procedure, the minute size of the implants, and the characteristic placement area, the patient can enjoy a light meal an hour after having the mini implants placed. With Mini Dental Implants, less bone is necessary, which is a great benefit for patients who have previously been told they would need bone grafts to receive any dental implants. Mini Dental Implants are surprisingly affordable, at a fraction of the cost of traditional implants. It is safe, biocompatible and provides an improved method of tooth replacement. Mini dental implants clearly represent an enormous breakthrough for the dental implant specialty as the most patient-friendly, cost- effective, proven dental implant system available today. Key Words: Mini Dental Implants, endosseous, titanium Introduction Dental Implant therapy has been one of the most significant advances in dentistry in the past 25 years. Endosseous dental-implant rehabilitation can provide partially or completely edentulous patients with function and esthetics similar to natural dentition while preserving adjacent teeth. (1–3) In clinical situations preserving adjacent teeth. (1–3) In clinical situations where residual dentitions are healthy and there are no systemic contraindications, dental-implant therapy may represent the highest standard of care for tooth replacement. Several different types of implants and restorations are available. The problem is, many of them are expensive and require a long recovery. The options depend upon the amount of bone available, the patient’s general health, and restoration preference. Three general categories of implant diameters are available: the mini- implant (≈1.8 mm), the standard-sized implant (≈3.75 mm) and the wide-body implant (≈6.0 mm), with all sizes in between. Use of mini-diameter implants is increasing. (4-13) Some implant companies have recognized the challenge of minimal bone presence and made implants of a smaller diameter (ranging from 3 to 3.5 mm). Although this change is only a slight reduction in diameter, it has allowed easier placement of root-form implants in the maxillary lateral incisor area, mandibular anterior sites or in any area in which bone has shrunken. These slightly smaller-diameter implants have been used widely and have been successful, in spite of allegations that they would be too weak. Mini Dental Implants are titanium screws that replace the root of a tooth. The ball shaped head and collar design can be used for both permanently cemented crowns or bridges as well as securing full or partial dentures. MDI, the mini dental implant system, FDA approved procedure is available at a fraction of the cost of traditional implants. Mini Dental Implants are constructed out of the same titanium alloy as the larger size traditional implants. Since the mini dental implant is a solid screw, a traditional implant is hollow in the center, it can be around half the size of a regular dental implant and just as strong. With the growing marketplace for dental implants and the advent of new technologies, implant design principles can affect success of immediately loaded implants. In 2006, Wang et al. (14) provided a definition based on a consensus from the International Congress of Oral Implantologists in which immediate loading was described as a technique in which the implant IJCD • JUNE, 2011 • 2(3) 89 supported restoration is placed into functional occlusal where residual dentitions are healthy and there are no systemic contraindications, dental-implant therapy may loading within 48 hours of implant insertion. © 2011 Int. Journal of Contemporary Dentistry described as a technique in which the implant supported restoration is placed into functional occlusal loading within 48 hours of implant insertion.
MINI DENTAL IMPLANTS
Mini dental implants are sometimes referred to as MDIs or small diameter implants (SDIs) or narrow body implants (NBIs). The narrow diameter or mini-implants are endosseous implants made of titanium alloy and less than 3 mm in diameter. They were introduced commercially to the dental profession in the 1990s and were first used for transitional prosthesis support. (15- 16) Late in l997, Dr. Sendax collaborated about his mini implant theory and design concepts with a colleague, Dr. Ronald A. Bulard who wasalready manufacturing and marketing standard sized dental implants, abutments, and other dental products. These so-called “mini”-diameter implants have been used successfully as interim implants to support provisional prostheses, while larger-diameter implants were integrating into bone. When minis were used as interim implants, the intent was to remove the mini- implants when the larger-diameter implants were put into service. As might have been anticipated, when attempting to remove these interim mini-implants, practitioners found that they could not be removed, because they had integrated into the bone during the interim service period. The pull-out strength of endosseous implants may be based on the length rather than the diameter of the implant,(17) and histologic analysis has shown that mini implants undergo osseointegration comparable to that of larger-diameter implants.(18) These findings have led some clinicians to advocate the use of mini implants to support and/or retain definitive prostheses.(19-21) Some small diameter implants are used as anchors for orthodontic use and are called TADs or temporary attachment devices. These differ from the more common mini implants in that they are removed after they are no longer needed and orthodontic treatment is completed.
DESIGN OF MINI DENTAL IMPLANTS
The design variations allow for use of the implants in the different densities of bone found throughout themouth. The body connects the tip with the prosthetic head and can be a parallel sided cylinder or a progressively tapered cone. Mini dental implants have a diameter of 1.8mm to 2.9mm and are available in various lengths. Multiple tip, thread, body and head designs are available across the category as well. Most tip designs are sharp or slightly blunted to provide self tapping ability of the implant through the medullary bone. It takes the form of a slim titanium rod with a retaining fixture that can be incorporated into a denture. The head of the implant is shaped like a ball: the retaining
REVIEW
attachment contains a rubber ‘O-ring’ that acts like a socket. This ‘O-ring’ holds a denture in place by snapping over the ball on the top of the implant. This enables the denture to rest easily on top of the gum tissue. The ball shaped head and collar design can be used for both permanently cemented crowns or bridges, as well as securing full or partial dentures. When used for fixed or cemented applications the prosthesis is cemented directly to the head of the implant. If the implant is to be used for a removable denture then a housing with a rubber gasket is attached to the acrylic denture and functions like a button that snaps on and off the implant. The denture sits snugly against the gums and is retained securely, allowing better chewing function and increased confidence. Because of the unique procedure, the size of the implants, and the characteristic placement area, the typical MDI patient can enjoy a light meal an hour or so after having the mini implants placed. A denture patient who has had his or her prosthesis stabilized with MDI can remove and replace the denture easily after a little practice, and can then easily utilize good dental hygiene. Mini Dental Implants are available in four lengths, 10, 13, 15 & 18 mm’s.
Procedure
The procedure is quicker and also non-invasive than that for a normal implant. Due to their size, they can cause little or no discomfort and are placed gently in the jawbone. A small pilot bit is used to create the opening for the implant to be threaded into the bone. Due to the size of the implant, the dentist will use a small ‘finger driver’ or screwdriver to help with the insertion. Ratchet wrench is used to secure the implant in place. Using such a minimally invasive procedure means the patient can heal faster, have less discomfort, and can use the implant much sooner. A regular implant is placed much differently. It requires a full flap of gum must be pushed back to see the bone. The bone is then removed with a series of burs to create space for the dental implant to be inserted. Most of this surgery can be avoided with a mini dental implant. Interim bis-acrylic composite crowns are fabricated with an indirect technique and cemented on the same day using provisional cement. The interim crown is kept out of occlusion, with minimal interproximal contacts. This approach is defined as nonfunctional immediate loading. (22) These interim crowns are meant merely for esthetics rather than function . The patient is provided with home care instructions and discharged. Ten days after surgery, the patient is recalled for evaluation. The definitive implant supported crowns are usually delivered within 2 weeks of surgery, which is considered to be immediate or immediate-delayed occlusal loading. (22) In 2006, Wang et al.(14) provided a definition based on a consensus from the International Congress of Oral Implantologists in which immediate loading was described as a technique in which the implant supported restoration is placed into functional occlusal loading within 48 hours of implant insertion. Furthermore, a distinction was made between the immediate restoration for aesthetic purposes, in which the restoration was placed out of occlusal contacts, and true immediate loading. When complications do arise with mini dental implants, the typical treatment is to move the mini implant to an adjacent spot. Because no bone is removed, the small opening in the gum closes and the body will fill in the defect with new bone.
INDICATIONS
Mini dental implants are much more than a solution for loose lower dentures.
They can be used virtually anywhere in the mouth.
They can have been used to:
1. Secure Upper and Lower Dentures
2. Replace a Single Missing Tooth
3. Replace Multiple Missing Teeth
4. Get rid of a Denture entirely and replace it with fixed Porcelain Crowns
5. Get rid of a metal partial denture
Edentulous arches with minimal remaining bone in a facial-lingual dimension.(23) Many patients who have been edentulous for several years do not have enough remaining facial-lingual bone to place standard- diameter implants without grafting. It is possible to place some mini-diameter implants (≈1.8 mm) in bone that is as narrow as 3 mm in a facial-lingual dimension Removable partial dentures (RPDs), Kennedy Class I, II and IV. (23)When bilateral distal extension (Class I), unilateral distal extension (Class II) or anterior extension (Class IV) removable partial dentures are planned, it is common knowledge that the dentures will rock toward the respective edentulous areas when chewing. If at least 3 mm of facial-lingual bone and 10 mm or more of crestalapical bone are present in any of the edentulous sites, and mini-implants are placed, patient satisfaction is increased significantly. The partial denture rests on the small implants, retained and supported in various ways: denture soft liner, rubber “O” rings in housings or other special abutments. Rocking toward the edentulous areas is eliminated and denture retention is improved. Extra support and retention under fixed partial dentures (FPDs). (23)Occasionally, situations arise in which an FPD is planned that has questionable potential retention from natural teeth, and the patient has refused RPD treatment or grafting and standard implants. Mini-implants can be placed in the edentulous areas and used to support the pontic areas of the FPD. When an FPD becomes loose on one end, and the prosthesis can be removed from the other abutment without destroying it, the prosthesis often can be salvaged. A small-diameter implant is placed in the pontic area, a hole is cut in the underside of the pontic, the abutment retainers of the FPD are cleaned and roughened internally, and the FPD is re-cemented using the mini-implant as additional support and retention under the pontic. The ideal candidate is one in good general and oral health. The best candidates have healthy gum tissues that are free of periodontal disease since the mini- implants are intimately connected with the gum tissues and underlying bone in the mouth, according to the American Dental Association (ADA). Individuals with uncontrolled diabetes are poor risks. Exclusion criteria for patients were conservative: severe or recent cardiac pathology, severe hypertension, uncontrolled diabetes, or bleeding disorder, AIDS, any condition that seriously compromised bone healing potential or autoimmune response, intravenous bisphosphonates, heavy smoking, personality disorder or psychosis, substance abuse, and physician veto. Although limited mesiodistal edentulous spaces contraindicate the placement of standard diameter implants, mini implants would also normally be contraindicated in locations with heavy lateral occlusal contacts.
ADVANTAGES / BENEFITS OF MINI-IMPLANTS:
Shatkin et al (24) carried out a retrospective evaluation of 2514 MDI implants in 531 patients over 5.5 years with a mean duration of 2.9 years. MDI 2.4 and 1.8mm diameter implants were placed to support removable full and partial upper and lower dentures, and fixed partial upper and lower dentures. There was an overall failure rate of 6% with significantly more implants failing in the maxilla than in the mandible; the average time to failure was 6.4 months. The authors considered that repeated forces of denture insertion and removal may have a tendency to disrupt the process of osseointegration however the overall implant survival rate was 94%. The authors commented that this rate of survival was likely due to the minimally invasive surgical approach which preserved the peri and endosteal blood supply. Flanagan (25) published a case report of three MDI implants placed in three mandibular extraction sockets and used to support a splinted fixed partial denture. The mini implants were immediately placed after extraction and allowed to heal for four months before fitting the lower partial denture. The case was followed for two years. The fixed partial lower denture was considered to be successful with no complications 91 IJCD • JUNE, 2011 • 2(3) © 2011 Int. Journal of Contemporary Dentistry reported. There was no apparent bone loss on radiograph and no clinical signs of inflammation or mobility. Histology studies Balkin et al (26) placed one MDI implant of 1.8mm diameter in each of two patients to act as transitional supporting implants for lower dentures. The MDIs were trephined out of the bone at four and five months. Histological evaluation showed that bone was in close adaptation to the MDI implant surfaces and vascular elements were apparent in the bone. The bone around the MDIs appeared to be healing, mature and well integrated into immediate function in the four to five month post-insertion period. The authors concluded that the MDI 1.8mm implant had the potential to become osseointegrated.
MAINTENANCE
Minis should be cleaned daily with a toothbrush and toothpaste. An electric brush may be used. In case of bridge or splinted crown installations, a water jet or floss threaders may be employed. Periodic follow -up visits will be scheduled to monitor mini implants, the fit of the dentures and the health of the gums. The O- rings will get loose and will need to be replaced because they do wear out. The more often that the patient removes and replaces his dentures, the more frequently he will need to come in to the office and have the o-rings replaced.
Discussion
The MDI is a one-piece implant that does not require a separate abutment. This simplifies the restorative phase resulting in a reduced cost for the patient. The MDI implant is made of a titanium-aluminum-vanadium alloy for increased strength. The MDI was initially designed for temporary prosthetic stabilization during the healing phase of standard implants (27). The MDI is also used for orthodontic anchorage (28) and temporary fixation of transplanted teeth (29). Its success in these procedures has led to its use in long term fixed and removable dental prostheses (30-32). Conventional implant treatment requires adequate bone width and interdental space. Augmentation procedures can be used to overcome these problems (33) but these techniques are complex and can cause post-operative pain and discomfort for the patient as well as incurring additional costs. The mini dental implant can be used in many such cases to overcome these kinds of limitations (34). Although the mini dental implant has a reduced surface area compared with a conventional endosseous implant (34) histology has shown that the MDI implant undergoes osseointegration . The percentage bone to implant contact for MDI is comparable to conventional implants (35). The narrow diameter of the MDI allows a
REVIEW
simplified insertion technique involving placement without raising a flap and immediate loading (35). Suggested indications for use for MDI include patients with inadequate bone width; older or medically compromised patients who would benefit from the preservation of blood flow to the implant area as a result of the flapless insertion technique; patients who wish to avoid extensive bone augmentation treatment. The relatively low cost of MDI enables the clinician to offer this treatment option to more patients (23, 30 ). The minimally invasive surgical insertion technique with the MDI brings greater postoperative comfort and decreased morbidity for the patient, allowing patients with health problems that preclude extensive surgical procedures the option of an implant (33). This ease of placement of MDI is considered to be a safety factor in its use (30), the ability to avoid flap surgery aids in healing as the periosteum is left undisturbed (36,37). Gingival healing is typically seen in 2 to 5 days (30). After placement of the MDI a patient can have an immediate temporary denture fitted. An extended healing period with MDI is usually not necessary (33). The pull-out strength of an implant has been shown to be based on its length rather than its diameter (38). The surface area of five MDI implants is considered to be equivalent to two traditional 3.75mm implants of equal length (30). In the edentulous arch multiple mini dental implants are considered to be more stable than two standard implants. The arch distribution of multiple MDI’s will better offset any fulcrum or tipping problems that can occur with two conventional implants positioned at the canine area (30). The MDI mini dental implant is available with either an O-ball head for use with removable or fixed dentures, or a square head for fixed prostheses or retrofitting a poorly adapted partial denture (16). The O-ball is considered to act as a shock absorber (39). The MDI is manufactured as a standard thread 1.8mm diameter, and with a modified thread and 2.4mm diameter. It comes in four lengths – 10mm, 13mm, 15mm and 18mm. The clinician should always select the longest possible MDI for the available bone to maximize stability (40). An absence of excessive micromotion at the bone-implant interface is required to enable the osseointegration process (41-43). It is thought that there is a critical threshold of micromotion above which a fibrous encapsulation process occurs rather than osseointegration (44) possibly around 100μ (42).
Conclusions
Mini implants are indicated for areas where the use of narrow diameter implants (3.0 mm) are contraindicated. Until long-term longitudinal clinical data on mini dental implants are unavailable, their use should be limited to areas with potentially less occlusal load.
113 MDI ClinicalStudies from AroundTheWorld
2016 Lisbon, Portugal
Small-Diameter Implants for Definitive Prosthodontic Treatment – 2016
A Literature Review
Lisa Steinhausen
Mestrado Integrado em Medicina Dentária
Universidade of Lisboa
http://repositorio.ul
.pt/bitstream/10451
/26156/1/ulfmd06020
_tm_Lisa_Steinhausen
Abstract
Introduction:
Dental implants are available in a wide range of diameters. Although there is still no clear definition, in this review small-diameter implants (SDIs) were considered ≤3.5mm in width. SDIs are mainly used when the placement of a larger implant is difficult due to insufficient bone substance. Due to structural weakness and a smaller contact area with the bone, they have been associated with biomechanical risk factors, especially in high occlusal loads, which might lead to peri-implant bone resorption or fatigue fracture of the implant.
Their survival and success rates in short- term follow-up seem to be comparable to regular-diameter implants (>95%).
The aim of this study was to review the survival and success rates of SDIs in definitive prosthetics, and report complications and failure reasons associated.
Materials and Methods:
An electronic search was undertaken in the PubMed database until March 2016, for small-diameter, narrow-diameter and mini implants with a diameter ≤3.5mm, used for definitive prosthetics with a follow-up time after loading of ≥1month.
Results:
The electronic search resulted in 907 publications and
79 met the eligibility criteria.
The MEAN SURVIVAL RATE was 95,2% with a mean follow-up time of 2,7years (6weeks to 12years).
Most common failures were of early biological origins. Complications were biologic or prosthetic related. SDIs were mainly inserted in anterior regions of the mandible or both jaws, restored with overdentures or fixed single restorations, following a one-stage surgical approach and immediate loading protocols.
Conclusion:
Within the limitations of this review,
the SURVIVAL of SMALL-diameter implants can be considered COMPARABLE to REGULAR-diameter implants in a short-term follow-up.
More randomized clinical trials (RCT’s)with longer follow-up times are necessary to confirm the long-term survival of SDIs. SDIs seem to have a LOW FRACTURE RATE within their range of indications, showing higher biological failures. Early biological failures could be related to the high incidence of immediate loading protocols, however more research is necessary to address these speculations. More research is also necessary to study the SDIs behavior in different loading protocols especially considering different restoration types, as well as to investigate their behavior in higher occlusive demanding situations, such as posterior locations.
114 MDI ClinicalStudies from AroundTheUSA
Newport Beach , Calif.
The Small-Diameter Implant: A Valuable Treatment Option for Many Patients
article by
Raymond Choi, DDS
GlidewellLab
Small-diameter implants (SDIs) are ideal for many patient types, providing an enriched quality of life for those who suffer from loose dentures or missing teeth but are unable to receive conventional implant therapy. With the exception of their distinctive diameters, SDIs are virtually identical to conventional-sized implants. The FDA has established 3.0 mm as the dividing line, with 3.0-mm diameter and above recognized as conventional implants, and 1.8–2.9 mm considered to be small-diameter. Like their traditional counterparts, SDIs are constructed from titanium alloy, exhibit precisely designed thread patterns, feature a surface treatment that supports osseointegration, and can be placed in an efficient, predictable and minimally invasive manner.
Additionally, SDIs appear to mirror the performance capabilities of conventional-sized implants.
According to multiple studies that measured the clinical outcomes of SDIs from five to 12 years, SDIs exhibit HIGH LONG-TERM SUCCESS rates.1-4
More studies will be helpful in developing and improving their diverse applications.
Although less frequently performed, SDIs may be placed to support a FIXED, ,splinted bridge connected to adjacent conventional-sized implants (Fig. 13).
For example, if one or more sites have ample bone width, regular-sized implants can be placed. If the adjacent area has compromised bone width that cannot accommodate conventional-sized implants without performing grafting or creating a cantilever pontic, a small-diameter implant may be placed instead (Fig. 14). Then, the clinician can splint the SDIs and conventional implant together with a fixed bridge.
Conclusion
FDA-cleared for long-term use, SDIs can frequently aid patients who would not otherwise receive implant treatment. These individuals may have given up hope because they needed bone grafting or a very expensive treatment that they couldn’t afford, or their health could not accommodate an invasive surgical procedure. With small-diameter implants, many patients can enjoy immediate improvement in their quality of life. It’s a rewarding experience for general dentists and a life-changing experience for patients, who express their gratitude and satisfaction instantly and commonly refer their family and friends. Because of the very simple surgical protocol that takes significantly less time than conventional implants, it’s one of the most productive and profitable procedures in my office. SDIs are a valuable and indispensable tool to add to any general dental practice.
115 MDI ClinicalStudies from AroundTheWorld
2017 Boston,USA
São Paulo,Brazil
Narrow‐ and regular‐diameter implants in the posterior region of the jaws to support single crowns: A 3‐year split‐mouth randomized clinical trial 2017
André Barbisan de Souza Flávia Sukekava Livia Tolentino
https://online
library.wiley.
com/doi/full/
10.1111/clr.
13076
Abstract
Objectives
The objective of this 3‐year split‐mouth randomized controlled clinical study was to compare narrow‐diameter implants (NDIs) to regular‐diameter implants (RDIs) in the posterior region of the jaws (premolars and molars) in regards to (i) the marginal bone level (MBL) and (ii) implant and prosthesis survival and success rates.
Material and Methods
A total of 22 patients were included in the study. Each patient received at least one implant of each diameter (Ø3.3 and Ø4.1 mm), placed either in the maxilla or mandible to support single crowns. A total 44 implants (22 NDIs and 22 RDIs) were placed and included in the study. Twenty‐one implants were placed in the premolar, whereas 23 were placed in molar areas. Radiographic evaluations to access the MBL were performed immediately after implant placement, 1 and 3 years after implant loading. Peri‐implant clinical variables including probing pocket depth (PPD) and bleeding on probing (BoP) were obtained after crown delivery, 1 and 3 years after loading. Furthermore, the survival and success rates of the implants and prosthesis were also evaluated.
Results
Twenty patients were able to complete the study. There was no statistically significant difference regarding MBL between groups at implant placement (p = .084), 1‐year (p = .794) and 3‐year (p = .598) time intervals. The mean peri‐implant bone loss at 3‐year follow‐up was −0.58 ± 0.39 mm (95% CI: −0.751 to −0.409) and −0.53 ± 0.46 mm (95% CI: −0.731 to −0.329) for NDIs and RDIs, respectively. BoP was present at 15% and 10% of NDIs and RDIs, respectively, at 3‐year follow‐up. PPD >5 mm was observed in 5% and 0% of the implants of NDIs and RDIs, respectively, at 3‐year follow‐up. At the 3‐year examination, the implant success rates were in the NDIs and RDIs sites, respectively, 95% and 100%. The corresponding values for prosthesis success rates were 90% for NDIs and 95% for RDIs.
Conclusion
The present study demonstrated that NDIs placed to support single crowns in the posterior region did NOT DIFFER to RDIs in regards to MBL, implant survival, and success rates.
116 MDI ClinicalStudies from AroundTheWorld
2014 Maringá -Paraná – Brazil
Narrow Diameter Implants Compared to Regular Diameter Implants Installed in the Posterior Region of the Jaws-Results from One-Year Follow Up 2014
De Souza Tolentino L, Garcez-Filho J, Tormena M, Lima LA and Araújo MG*
State University of Maringá -Paraná – Brochure
Dentistry, an open access journal
Volume 4 • Issue 6 • 1000236
Abstract
Purpose: The aim of this prospective clinical study was to analyze marginal bone loss around Narrow Diameter Implants (NDIs) in comparison with that of Regular Diameter Implants (RDIs) installed in the posterior region of the jaws after one year of loading with single prostheses.
Material and Methods:
A total of 21 patients with a mean age of 57.2 years were included in the study. The patients received one implant of each diameter in the maxilla or in the mandible. Panoramic radiographs were realized immediately after prostheses installation (T0) and one year after loading (T1). Measurements were performed from implant shoulder to the first point of bone/implant contact. The differences in marginal bone change between the groups were analyzed by Student t-test for paired samples. A level of 95% of significance was adopted.
Results:
A total of 42 implants were installed (21 RDIs and 21 NDIs). At the end of the follow-up period (12 months of loading), implant success and survival rates of 100% were observed. The bone loss around implants at T0 was 0.41 (± 0.45) mm for NDIs and 0.47 (± 0.60) mm for RDIs and at T1 was 1.3 (± 0.3) mm for NDIs and 1.24 (± 0.3) mm for RDIs. No statistically significant differences between the groups were found (p>0.05).
Conclusion:
This study demonstrated that RDIs and NDIs produced SIMILAR marginal bone alterations patterns after one year of loading, regardless the implant location, indicating that NDIs may be used in the posterior region of the jaws with single unit prostheses in selected patients. Keywords: Narrow diameter; Dental implants;
117 MDI ClinicalStudies from AroundTheWorld
Montreal, Quebec,Canada
São Paulo, Ribeirão Preto, SP Brazil
Osseointegration of standard and mini dental implants: a histomorphometric comparison 2017
Jagjit S. Dhaliwal, Rubens F. Albuquerque, Jr, […], and Jocelyne S. Feine
Jagjit S. Dhaliwal,1 Rubens F. Albuquerque, Jr,2 Monzur Murshed,1,3 and Jocelyne S. Feine1
1Faculty of Dentistry, McGill University, 2001 McGill College Avenue, Suite 500, Montreal, Quebec H3A 1G1 Canada
2Faculty of Dentistry of Ribeirão Preto, University of São Paulo, Ribeirão Preto, SP Brazil
https://www.ncbi
.nlm.nih.gov/pmc/
articles/PMC5411366/
Abstract
Background
Mini dental implants (MDIs) are becoming increasingly popular for rehabilitation of edentulous patients because of their several advantages. However, there is a lack of evidence on the osseointegration potential of the MDIs. The objective of the study was to histomorphometrically evaluate and compare bone apposition on the surface of MDIs and standard implants in a rabbit model.
Methods
Nine New Zealand white rabbits were used for the study to meet statistical criteria for adequate power. Total 18 3M™ESPE™ MDIs and 18 standard implants (Ankylos® Friadent, Dentsply) were inserted randomly into the tibia of rabbits (four implants per rabbit); animals were sacrificed after a 6-week healing period. The specimens were retrieved en bloc and preserved in 10% formaldehyde solution. Specimens were prepared for embedding in a light cure acrylic resin (Technovit 9100). The most central sagittal histological sections (30–40 μm thick) were obtained using a Leica SP 1600 saw microtome. After staining, the Leica DM2000 microscope was used, the images were captured using Olympus DP72 camera and associated software. Bone implant contact (BIC) was measured using Infinity Analyze software.
Results
All implants were osseointegrated. Histologic measures show mineralized bone matrix in intimate contact with the implant surface in both groups. The median BIC was 58.5 % (IQR 8.0) in the MDI group and 57.0 % (IQR 5.5) in the control group (P > 0.05; Mann-Whitney test). There were no statistical differences in osseointegration at 6 weeks between MDIs and standard implants in rabbit tibias.
Conclusions
Based on these results, it is concluded that osseointegration of MDIs is SIMILAR to that of standard implants.
Keywords: Bone implant contact, Mini dental implant, Osseointegration
Background
The term “osseointegration” was first introduced to explain the phenomenon for stable fixation of titanium to bone by Brånemark et al. in the 1960s [1]. Osseointegrated implants were introduced, a new era in oral rehabilitation began, and many studies were conducted [2, 3]. A success rate of over 90% has been reported [4, 5]. Further, a success rate of 81% in the maxillary bone and 91% in the mandible can be accomplished [6]. Dental implants have been widely used for the stabilization of complete dentures and also help to maintain bone, function, esthetics, and phonetics and improve the oral health-related quality of life [7]. The dental implants are available with different surfaces and sizes. The size of the dental implants usually ranges in the diameter range of 3 mm (narrow diameter) to 7 mm (wide diameter). However, majority of the implants fall in the “standard diameter” range of 3.7 to 4.0 mm [8]. Mini dental implants or small size implants are also being widely used for stabilizing the complete dentures [9], for orthodontic anchorage [10–12], single tooth replacements [13, 14], fixing the surgical guides for definitive implant placement [15], and as transitional implants for the support of interim removable prosthesis during the healing phase of final fixtures [16, 17]. The single-piece mini dental implants (MDIs) are becoming increasingly popular for the purpose of denture stabilization. There are many advantages of the MDIs over the regular implants. The surgery is minimally invasive as compared with conventional implant surgery which helps in decreased morbidity for the patient. Transmucosal placement is possible using a single pilot drill, and these can often be loaded immediately [18]. Gingival healing is typically seen in 2 to 5 days, extended healing period with MDIs is usually not necessary [19]. The insertion of MDIs needs a minimal disturbance of the periosteum, thus osseointegration process is accelerated and time needed for MDIs tends to be considerably small than that of regular implants due to less injurious insertion procedure [9]. The need for sutures or long recovery periods is eliminated [3]. The patient can walk in to the office in the morning and is out the same day with a full set of teeth, the patient is allowed to eat the same day. These can work well for patients who have significant bone loss that restrict them from being a candidate for regular dental implants. MDIs are also a solution for patients that cannot have surgery for medical reasons. MDIs are also cost effective [20]. Considerable confusion exists in the literature regarding the best method to monitor the status of a dental implant. Various methods have been used to demonstrate the osseointegration of dental implants. A common and time-tested method to evaluate biological responses to an implant is to measure the extent of bone implant contact (BIC), referred to as histomorphometry at the light microscopic level. Bone implant contact (BIC) is one of the parameters which has been used extensively to study the amount of bone apposition next to the implants [21–27]. When an implant is placed in the jaw, it is in contact with compact bone as well as cancellous bone. The different structures of the two types of bone frequently result in variation of mineralized bone-to-implant contact length along the implant surface [28, 29]. Albrektsson et al. identified the key features affecting osseointegration about 4 decades ago, e.g., implant surface and topography, surface chemistry, charge, and wettability [30]. Roughness and enhanced surface area seems to be helpful for osseointegration. Carlsson et al. reported that screw-shaped implants with a rough surface had a stronger bonding than implants with a polished surface [31]. A coarse surface seems to be more appropriate for osseointegration of implants than a relatively smoother implant surface by representing a greater degree of implant integration [32–34]. The bone contact areas of 3M™ESPE™ MDIs are surface treated. The treatment process of these MDIs includes sandblasting with aluminum oxide particles followed by cleaning and passivation with an oxidizing acid [35]. Despite the advantages of the mini dental implants, evidence on their efficacy and long-term success is lacking. The success of these implants will depend on their union with the surrounding bone. New implant systems entering into the market have to be studied with the help of animal models first, to demonstrate the osseointegration potential for their probable success in humans. There is a limited evidence regarding the 3M™ESPE™ MDIs. Therefore, there is a need for an animal study to explore the osseointegration of these implants to assist in better understanding of the treatment selection, prognosis, and outcomes for the patients.
118 MDI ClinicalStudies from AroundTheUSA
New York,NY 2017
Narrow-diameter implants: A solution for replacing single missing lower incisors
September 12, 2017
By Peter Mann, DDS, FICOI, FAGD
The Perio ImplantAdvisory
Most dentists dread having to replace single missing mandibular incisors due to the numerous challenges involved. Peter Mann, DDS, FICOI, FAGD, presents two case studies demonstrating the successful use of narrow-diameter implants (mini-implants) for patients who “don’t want a bridge” and those who were told they are not candidates for conventional dental implants.
MOST DENTISTS DREAD THE THOUGHT of replacing a single missing mandibular incisor. Numerous challenges make this procedure unappealing. There’s usually not enough space for a regular dental implant due to mesiodistal restrictions; roots on either side don’t allow enough space for implant placement. There are buccolingual restrictions as well, since the ridge frequently atrophies in the anterior of the lower mandible. Placing a bridge would involve prepping a lower incisor for an implant abutment. As we all know, these are the weakest and smallest teeth in the mouth. Lower incisors make for poor long-term abutments, and the prognosis is usually guarded. The last option is a removable prosthetic. Whatever you call it—flipper, flexi, partial denture—one thing is for sure, the patient can lose it, break it, and/or not be satisfied with it. Interestingly, patients have begun to actively seek out narrow-diameter implant treatment and have found my office, since many general dentists and specialists do not offer this option. Patients present with the chief complaint of “I don’t want a bridge” and have been told that they are not conventional dental implant candidates. My previous article on “Narrow-diameter implants in the esthetic zone” presented several cases explaining how these types of implants can be used in challenging cases involving the anterior esthetic zone. In this article, I will present two cases that demonstrate the successful use of narrow-diameter implants (mini-implants) for the replacement of missing lower incisors.
Case No. 1
This is the case of a patient who has been missing a lower incisor for more than a year due to a failed root canal treatment (RCT). While there’s plenty of space mesiodistally, bone sounding helped us determine that there was only 4 mm of bone in the buccolingual dimension. A mini-implant was placed without raising a flap, the impression was taken at the time of surgery, and the implant was restored three weeks later.
Case No. 2
This patient presented with discomfort and mobile teeth Nos. 24 and 25. Extractions were performed, and the area was allowed to heal for six months. Mini-implants were placed in site Nos. 24 and 25 and immediately loaded with temporary crowns. The final splinted restoration was cemented two weeks later.
Conclusion
Placing narrow-diameter dental implants to replace missing incisors can overcome many of the traditional challenges facing clinicians. Patients with thin ridges and narrow spaces between roots can be restored without using fixed partial bridges or removable prosthetics.
MORE ARTICLES BY DR. PETER MANN …
Deciding between pink porcelain versus ridge augmentation in the esthetic zone Learning from root canal complications A cost-effective method of creating a dental implant surgical guide for ridge augmentation Step-by-step procedure to simplified and efficient root canal techniques Dental implants: The importance of patient compliance with immediate loading
Peter Mann, DDS, FICOI, FAGD, graduated from the New York University College of Dentistry in 2008, and completed his general practice residency at Kings County Hospital in 2009. He is the director of Smile Arts of NY, a comprehensive general practice in midtown Manhattan with an emphasis on cosmetic and implant dentistry.
119 MDI ClinicalStudies from AroundTheWorld
Paris,France
Impact of implant length and diameter on survival rates. 2006
Authors
Renouard F1, Nisand D.
Author information
1
Private Practice, 26 Avenue Kléber, 75116 Paris, France. franck@renouard.net
Citation
Clin Oral Implants Res. 2006 Oct;17 Suppl 2:35-51.
https://www.ncbi.nlm
.nih.gov/m/pubmed/
16968380/?i=3&from
=/24316701/
Abstract
INTRODUCTION: Despite the high success rates of endosseous oral implants, restrictions have been advocated to their placement with regard to the bone available in height and volume. The use of short or nonstandard-diameter implants could be one way to overcome this limitation.
MATERIAL AND METHODS: In order to explore the relationship between implant survival rates and their length and diameter, a Medline and a hand search was conducted covering the period 1990-2005. Papers were included which reported: (1) relevant data on implant length and diameter, (2) implant survival rates; either clearly indicated or calculable from data in the paper, (3) clearly defined criteria for implant failure, and in which (4) implants were placed in healed sites and (5) studies were in human subjects.
RESULTS:
A total of 53 human studies fulfilled the inclusion criteria. Concerning implant length, a relatively high number of published studies (12) indicated an increased failure rate with short implants which was associated with operators’ learning curves, a routine surgical preparation (independent of the bone density), the use of machined-surfaced implants, and the placement in sites with poor bone density. Recent publications (22) reporting an adapted surgical preparation and the use of textured-surfaced implants have indicated survival rates of short implants comparable with those obtained with longer ones. Considering implant diameter, a few publications on wide-diameter implants have reported an increased failure rate, which was mainly associated with the operators’ learning curves, poor bone density, implant design and site preparation, and the use of a wide implant when primary stability had not been achieved with a standard-diameter implant. More recent publications with an adapted surgical preparation, new implant designs and adequate indications have demonstrated that implant survival rate and diameter have no relationship.
DISCUSSION:
When surgical preparation is related to bone density, textured-surfaced implants are employed, operators’ surgical skills are developed, and indications for implant treatment duly considered, the survival rates for short and for wide-diameter implants has been found to be comparable with those obtained with longer implants and those of a standard diameter. The use of a short or wide implant may be considered in sites thought unfavourable for implant success, such as those associated with bone resorption or previous injury and trauma. While in these situations implant failure rates may be increased, outcomes should be compared with those associated with advanced surgical procedure such as bone grafting, sinus lifting, and the transposition of the alveolar nerve.
PMID 16968380 [Indexed for MEDLINE]
120 MDI ClinicalStudies from AroundTheWorld
Valencia, Spain
Narrow-diameter implants: are they a predictable treatment option?
A literature review.
2014
Review article
Sierra-Sánchez JL, et al. Med Oral Patol Oral Cir Bucal. 2014.
https://www.ncbi
.nlm.nih.gov/pmc/
articles/PMC3909436/
Abstract
OBJECTIVE:
To evaluate the predictability of narrow-diameter implants as a treatment option in routine clinical practice. A literature review was performed of studies reporting clinical results obtained with these implants. Survival rates, peri-implant bone loss and related complications were evaluated. The working hypothesis was that narrow-diameter implants offer clinical results similar to those obtained with implants of greater diameter.
Introduction
Treatment with dental implants offers a predictable solution for most situations seen in routine clinical practice. However, bone availability is often a limiting factor in planning our treatments. A number of surgical techniques allow us to increase the available bone width, such as for example expansion with osteotomes (1), guided bone regeneration (2), autologous bone grafts (3), crestal expansion techniques (4), and osteogenic distraction (5,6). Although these procedures offer good results in implantology, they are not without complications (7,8). The associated inconven-iences are increased morbidity, longer healing times, and infection secondary to wound dehiscence or membrane exposure (9,10). In patients with deficient crest width, the utilization of narrow-diameter implants therefore constitutes a technically more simple treatment alternative. The definition of a narrow-diameter implant is subject to controversy. Although no universally accepted classification of implant diameters has been established to date, a narrow-diameter implant is generally taken to have a diameter of ? 3.0 mm and ? 3.5 mm. Some recent studies with narrow-diameter implants have reported implant success and survival rates similar to those obtained with greater diameter implants (11,12). However, few studies with prolonged periods of follow-up evaluating the predictability of these implants have been published. The objective of the present literature review is to evaluate the predictability of narrow-diameter implants as an alternative to other technically more complex procedures, based on the survival rates, changes in peri-implant bone height and related complications.
MATERIAL AND METHODS:
A Medline-PubMed search covering the period between 2002 and 2012 was carried out. Studies published in English and with a follow-up period of at least 12 months were considered for inclusion. A manual search was also conducted in different journals with an important impact factor. results: Twenty-one studies meeting the screening criteria were included in the literature review. A total of 2980 narrow-diameter implants placed in 1607 patients were analyzed.
CONCLUSIONS:
The results obtained from the literature indicate that narrow-diameter implants are a predictable treatment option, since they afford clinical results comparable to those obtained with implants of greater diameter.