Figure 1. VELscope examination. The clinician shines the blue excitation light into the patient’s oral cavity and looks through the Handpiece.

Figure 2. Illustration of VELscope’s principle of operation.
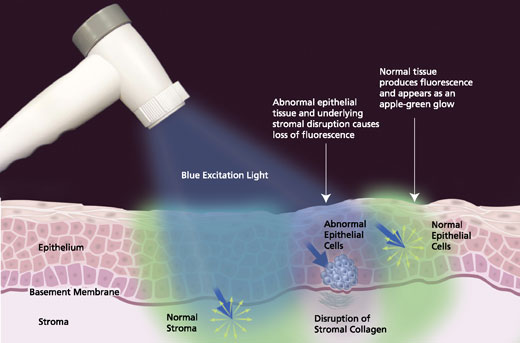
Figure 3. Representative examples of direct visualization under both white light and VELscope examination – photos courtesy of the British Columbia Oral Cancer Prevention Program.

No apparent lesion

Normal fluorescence pattern

Visible leukoplakia

Irregular, dark area visible under fluorescence visualization. Biopsy-confirmed severe dysplasia

No apparent lesion

Irregular, dark area visible under fluorescence visualization. Biopsy-confirmed Carcinoma in Situ (CIS)
Statistical Information
Every hour of every day in America someone dies of Oral Cancer. Oral Cancer is the sixth most commonly diagnosed form of cancer in the United States. Presently 30,000 patients are diagnosed annually with oral cancer. The 5-year survival rate is only 50%, accounting for 8,000 deaths each year. Oral Cancer risk factors include tobacco use, frequent and/or excessive alcohol consumption, a compromised immune system, past history of cancer, and the presence of the HPV virus. Recently however 25% of all newly diagnosed cases have been in patients under the age of forty with none of the known risk factors. Oral Cancer is one of the few cancers whose survival rate has not improved in the past 50 years. This is due primarily to the fact that during this time we have not changed the way we screen for this disease (a visual and manual examination of the oral cavity, head, and neck).
Oral Squamous Cell Carcinomas (OSCC) make up over 90% of all oral cancers, and because of their appearance, it has been difficult to differentiate them from the other relatively benign lesions of the oral cavity. Early OSCC and potentially malignant lesions can appear as a white patch (leukoplakia, as a reddened area (erythroplakia), or as a red and white (erythroleukoplakia) mucosal change under standard white light examination. However, these cellular changes are often non-detectable to the human eye (even with magnification eyewear) under standard lighting conditions. Often, when the lesion becomes visible, it has advanced to invasive stages. The high mortality rate is directly related to the lack of early detection of potentially malignant lesions. When diagnosis and treatment are performed at or before a Stage 1 carcinoma level, the survival rate is more than 90%.
The cancers which have seen a major decline in the mortality rate have included colon, cervical, and prostate cancer and the primary reason is early detection and screening.
We can make a difference in the oral cancer mortality rate.
Early screening, diagnosis, and treatment planning save lives.
Risk Factors
Understanding the causative factors of cancer will contribute to the prevention of the disease. Age is frequently named as a risk factor for oral cancer, as most of the time, it occurs in those over the age of 40. The age of diagnosed patients may indicate a time component in the biochemical or biophysical processes of aging cells that allows malignant transformation, or perhaps, immune system competence diminishes with age. However, it is likely that the accumulative damage from other factors, such as tobacco use, is the real culprit. It may take several decades of smoking, for instance, to precipitate the development of cancer. Having said that, tobacco use in all its forms is number one on the list of risk factors. At least 75% of those diagnosed are tobacco users. When you combine tobacco with heavy use of alcohol, your risk is significantly increased, as the two act synergistically. Those who both smoke and drink, have a 15 times greater risk of developing oral cancer than others.
Tobacco and alcohol are essentially chemical factors, but they can also be considered lifestyle factors since we have some control over them. Besides these, there are physical factors such as exposure to ultraviolet radiation. This is a causative agent in cancers of the lip, as well as other skin cancers. Cancer of the lip is one oral cancer whose numbers have declined in the last few decades. This is likely due to the increased awareness of the damaging effects of prolonged exposure to sunlight, and the use of sunscreens for protection. Another physical factor is exposure to x-rays. Radiographs were regularly taken during examinations, and at the dental office, are safe, but remember that radiation exposure is accumulative over a lifetime. It has been implicated in several head and neck cancers.
Biological factors include viruses and fungi, which have been found in association with oral cancers. The human papillomavirus, particularly HPV16 and 18, has been implicated in some oral cancers. HPV is a common, sexually transmitted virus, which infects about 40 million Americans. There are about 80 strains of HPV, most thought to be harmless. But 1% of those infected, have the HPV16 strain which is a causative agent in cervical cancer, and now is linked to oral cancer as well. There are other risk factors that have been associated with oral cancers but have not yet been definitively shown to participate in their development. These include lichen planus, an inflammatory disease of the oral soft tissues.
There are studies that indicate a diet low in fruits and vegetables could be a risk factor, and that conversely, one high in these foods may have a protective value against many types of cancer.
Signs & Symptoms
One of the real dangers of this cancer is that in its early stages, it can go unnoticed. It can be painless, and little in the way of physical changes may be obvious. The good news is, however, that your dentist or doctor can see or feel the precursor tissue changes, or actual cancer while it is still very small, or in its earliest stages. It may appear as a white or red patch of tissue in the mouth, or a small indurated ulcer that looks like a common canker sore. Because there are so many benign tissue changes that occur normally in your mouth, and some things as simple as a bite on the inside of your cheek may mimic the look of a dangerous tissue change, it is important to have any sore or discolored area of your mouth, which does not heal within 14 days, looked at by a professional. Other symptoms include; a lump or mass which can be felt inside the mouth or neck, pain or difficulty in swallowing, speaking, or chewing, any wart-like masses and hoarseness which! lasts for a long time, or any numbness in the oral/facial region. Other than the lips, the most common areas for oral cancer to develop are on the tongue and the floor of the mouth. Individuals that use chewing tobacco, are likely to have them develop in the sulcus between the lip or cheek and the soft tissue (gingiva) covering the lower jaw (mandible). In the US, cancers of the hard palate are uncommon, though not unknown. The base of the tongue at the back of the mouth, and on the pillars of the tonsils, are other sites where it is commonly found. If your dentist or doctor decides that an area is suspicious, the only way to know for sure is to do a biopsy of the area. This is not painful, is inexpensive, and takes little time. It is important to have a firm diagnosis as early as possible. It is possible that your general dentist or medical doctor may refer you to a specialist to have the biopsy performed. This is not cause for alarm, but a normal part of referring that happens! between doctors of different specialties.
Early Detection
Historically, it has been difficult to determine which abnormal tissues in the mouth are worthy of concern. The fact is, the average person routinely has conditions existing in their mouths that mimic the appearance of pre-cancerous changes, and very early cancers of the soft tissues. One study determined that the average dentist sees 3-5 patients a day who exhibit soft tissue abnormalities, most of which are benign in nature. Even the simplest things, such as a canker sore (herpes simplex), the wound left by accidentally biting the inside of your cheek, or sore spots from a poorly fitting prosthetic appliance or denture, all at first examination, share similarities with dangerous lesions. Some of these conditions cause physical discomfort, others are painless. The question is which ones deserve action, and which ones bear watching and waiting?
There has been a tendency to watch these areas over an extended period to determine if they are dangerous or not. Unfortunately, this philosophy leads to a situation in which a dangerous lesion may continue to prosper and grow into a later-stage, hard-to-cure cancer. Any sore, discoloration, induration, prominent tissue, irritation, or hoarseness, which does not resolve within a two-week period on its own, with or without treatment, should be considered suspect and worthy of further examination or referral. Besides a routine visit to the dental office for regular examinations, it is the patient’s responsibility to be aware of changes in their oral environment. When these changes occur, they need to be brought to the attention of a qualified dental professional for examination. The dental professional needs to be current in the knowledge base necessary to make a proper diagnosis and be competent in the proper screening procedures to identify oral cancer.
How to know if you have had a proper oral cancer screening
There are two separate issues, discovery, and diagnosis. Discovery is the result of a thorough visual and manual examination. A protocol for a comprehensive oral cancer screening appears elsewhere in this section of the website. It includes a systematic visual examination of all the soft tissues of the mouth, including the manual extension of the tongue to examine its base, a bi-manual palpation of the floor of the mouth, and a digital examination of the borders of the tongue, and the lymph nodes surrounding the oral cavity and in the neck. New diagnostic aids, including lights, dyes, and other techniques are beginning to appear on the marketplace. While making the discovery process more effective, it is still possible to do a comprehensive examination through a proper visual and tactile process.
Once suspect tissues have been detected, the only way a definitive diagnosis of oral cancer may be made is through biopsy. Given the large number of tissue abnormalities a dentist sees every day, it is not logical, nor practical, that each one of these is biopsied. The first question which may help in the determination of which abnormality bears closer examination, is how long has the suspect condition been present? Any condition that has existed for 14 days or more without resolution should be considered suspect and worthy of further diagnostic procedures or referral. Certainly, it is common knowledge that two of the most prevalent lesions that mimic oral cancer are herpes simplex ulceration, and aphthous ulcerations, each resolving of their own accord in approximately 10-14 days. Perhaps that sentence should be underlined since one of the most common diagnoses received with referred patients to a major university cancer pathology department is “an atypical herpetic! c/aphth ous lesion” These all too frequently turn out to be squamous cell carcinomas, which have been under observation…. for several months.
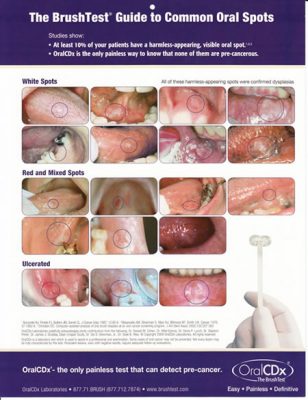
Still, it would seem impractical at these early timelines to engage in the biopsy. An oral biopsy brush is available that makes this decision to get an early diagnosis through biopsy easier to make. Simple, painless, and accurate diagnoses of soft tissue abnormalities can be obtained through its use.
Note that this system is not designed to provide the kind of information, specifically cellular architecture, that would be obtained through a punch or incisional biopsy. But it will provide an answer to the question of whether malignancy exists or not, through a quick, minimally invasive, and inexpensive procedure. Should positive results be returned through this system, the brush biopsy must be followed by a conventional biopsy procedure for confirmation. The strong argument for the brush biopsy is that it eliminates the waiting and watching of a suspicious lesion, while it develops from a highly treatable and curable, early-stage localized cancer, into a life-threatening late-stage malignancy. Positive identification of oral cancers at the earliest stages results in the best prognosis for a cure and long-term survivability.
Creating awareness, discovery, diagnosis, and referral. When it comes to oral cancer and saving lives, these are the primary responsibilities of the dental community. The most important step in reducing the death rate from oral cancer is early discovery. No group has a better opportunity to have an impact than members of the dental community.
An important message about oral cancer from the American Dental Association
Now precancerous cells can be detected years before oral cancer can start. See your dentist regularly and ask about a brush test for oral spots.
What You Can Expect as Part of Your Routine Exam:
- Your dentist and hygienist look for spots in your mouth.
- If a spot is observed, your dentist may recommend further testing.
- A brush test sample is then sent for computer-assisted laboratory analysis.
- Even if a lab identifies abnormal cells, they can typically be removed years before they can harm you.
If a brush test finds unhealthy cells, they can typically be removed, years before they can penetrate the basement membrane and become oral cancer.
What you should know:
- Most People Will Have tiny white or red spots in their mouth at one time or another.
- See your Dentist Regularly for a thorough oral exam. Although the vast majority of these spots do not contain unhealthy cells, your dentist may recommend further testing.
- Even If A Lab Identifies abnormal cells, they can then typically be removed years before they can harm you.
For more information please visit www.ada.org
ADA American Dental Association
America’s leading advocate for oral health
The OralCDx brand of brush test is an adjunct to the professional oral examination in the early detection of oral precancers. This test is not a substitute for a scalpel biopsy which should continue to be utilized to evaluate suspicious oral lesions. The ADA has no financial interest in this product. This brochure is part of educational programs supported by a grant from Oral Cancer Prevention International, Inc, provider of the ORalCDx brand of brush test. For more information please visit www.ada.org